
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Feature: Overcoming the Challenges of Difficult Acne Cases
Acne
| N |
early everyone suffers from acne at some point in life,1 and 20% of all patient visits to dermatologists are acne-related. Acne, a chronic disease, affects a majority of those 12 to 24 years of age and may continue to afflict some patients well into adulthood. The physiological, psychological, and quality-of-life impacts associated with acne are significant and well studied. The effective treatment of acne in sufferers of all ages and types is therefore critical.
Pathogenesis and Life Cycle of Acne
The pathogenesis of acne is multifactorial and involves the interaction of four processes. First, follicular keratinization is increased, which results in the follicles becoming plugged. There is an increase in sebum production, often related to increased hormone production, which contributes to the obstruction of the follicles. Propionibacterium acnes bacteria then proliferate in the obstructed follicles and cause the final process, the inflammatory and immune responses in the skin.
Acne, typically, is first diagnosed in adolescence with onset of hormonal changes associated with puberty. Excessive sebum is produced by these patients, which results in oily skin and, when combined with follicular hyperkeratinization, comedonal acne. The inflammatory reaction to these initial lesions leads to the formation of the papules, pustules, and nodules seen in more severe forms of acne.
The incidence of acne declines with age, but the disease may persist beyond adolescence. A recent study indicated the prevalence of adult acne at 3% in men and 12% in women. Hormonal fluctuations may influence the persistence or development of the disease in adult women. The type and severity of acne often differs by sex and age. Adult females are more likely than males to suffer from inflammatory acne that affects the lower face, whereas teenage males are more frequently affected by acne than teenage females. Thus, optimal treatment of acne vulgaris varies according to the age and sex of the patient, as well as the type and severity of disease.
Overview of Acne Treatment
The most effective acne treatments address the individual patient?s acne by targeting multiple pathogenic factors. For example, topical retinoids restore the normal follicular keratinization processes and reduce the formation of comedos; benzoyl peroxide (BPO) also is comedolytic. The production of sebum may be reduced by using the oral retinoid isotretinoin (Accutane, Amnesteem) or systemic hormonal agents (such as oral contraceptives) Antimicrobials, such as BPO and systemic antibiotic agents, reduce P. acnes counts and associated inflammation. The anti-inflammatory qualities of retinoids may also be used to control acne-related inflammation. Therapies should be initiated early to minimize or prevent the sequelae of acne, which include scarring and other psychological effects.
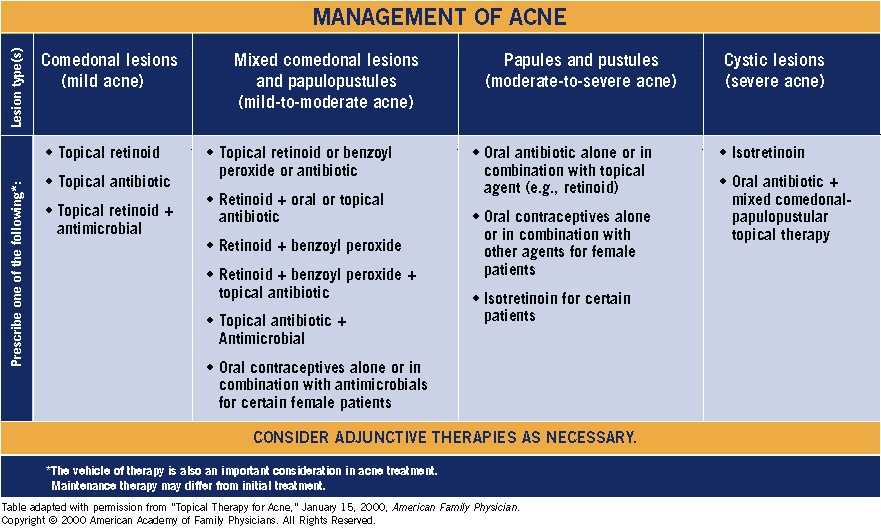
Because acne treatments vary according to their mode of action and their effectiveness against the key causes of acne, specific agents are used to target specific types of acne. A brief review of the important classes of anti-acne agents and how they are used to treat mild, moderate and severe acne is presented below (See Figure 1).
Figure 1: The management of acne varies by type of acne/lesion.(CLOSE WINDOW)
Topical retinoids. Topical retinoids, such as tretinoin (Avita, Renova, Retin-A, Solage, Tri Luma), adapalene (Differin) and tazarotene (Tazorac), are effective for the initial or early treatment of mild-to-moderate, non-inflammatory, comedonal acne when used alone. Retinoids can also be combined with antimicrobial treatments for inflammatory or more severe acne and used alone or in combination for long-term maintenance therapy.
Oral antibiotics. Oral antibiotics are most effective for inflammatory acne lesions, moderate-to-severe acne, and in patients where topical treatments have failed. Commonly used agents, such as tetracycline and erythromycin, are generally not used as monotherapy because their use may contribute to P. acnes resistance. Oral antibiotics also may have rare, but in some cases severe, side effects that may influence their use as acne therapy. For all of these reasons, these agents should be prescribed at therapeutic doses for the minimal effective time period, discontinued, and then followed by long-term topical therapy.The use of oral antibiotics in combination with BPOs or retinoids is also effective in minimizing P acnes resistance and maximizing efficacy.
Topical antibiotics. Topical antibiotics, such as clindamycin and erythromycin, are generally not recommended as monotherapy because they induce resistance in P. acnes, which results
in decreased efficacy. These agents are, however, highly effective acne treatments when used in combination with other agents, such as OCs and BPO.
Benzoyl peroxide. When used alone, this agent is an effective antimicrobial and has comedolytic activity.13,17,20 In combination with an antibiotic (e.g., 1% clindamycin/5% benzoyl peroxide), it is a well-studied, effective, well-tolerated treatment for inflammatory acne.20-22 Combination antibiotic/BPO therapies are effective when used with retinoids.
Hormonal Therapies. These therapies are now recognized as effective acne therapies in women with inflammatory acne or certain hormonal conditions. These women may benefit from treatment with OC products, such as ethinyl estradiol/levonorgestrel (Alesse, Levlen, Levlite, Plan B, Seasonale, Tri-Levlen, Triphasil) and drospirenone/ethinyl estradiol (Yasmin).1,5,23 Antiandrogens, such as spironolactone, also have anti-acne benefits and may be used alone or in combination with oral antibiotics or topical therapies for certain women.19
Oral retinoids. Isotretinoin is a mainstay therapy for severe, scarring acne and acne that relapses or is resistant to oral and topical therapies.5,14 Isotretinoin addresses all four of the pathophysiologic factors of acne and is a highly effective therapy; however, it has side effects that include teratogenic effects in pregnant women and reports of potential psychological impacts.1,5,14,17 These side effects limit its use in certain patients, such as women of childbearing age.1,5,17
Adjunctive therapies. Novel adjunctive treatments for acne include photodynamic therapy, light and laser procedures that target specific causes of acne.1,5 Blue light treatments, for example, kill P. acnes, whereas red light treatments are anti-inflammatory.1 Chemical and microdermabrasive procedures, as well as procedures that involve comedo extraction, also may be useful components of acne treatment programs.
Other Considerations
An equally important factor in determining treatment for acne is consideration of the vehicle used to deliver the active ingredient of a particular therapy. The emollient, humectant, or occlusive properties of the treatment vehicle are a key factor in maximizing the overall health of skin: repairing skin barrier function and improving hydration, for example, are critical components of effective acne therapy.22,24,25 Additionally, environmental factors must be considered when evaluating certain acne treatments, because they may affect efficacy.
Date: 2016-06-13; view: 720
| <== previous page | | | next page ==> |
| Equipment Cost Factors | | | Feature: Spotlight on Treating Inflammatory Acne |