
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Ñhàptår 6: Àppliñàtiîn Prîblåms
The most common is called jaundice nadpechenochnaya increased destruction of red blood cells - both mature cells and their precursors. Destruction of mature cells may be the result of hemolysis or effect of utilization of blood after internal bleeding, such as damaged soft tissues. Ineffective Erythropoiesis occurs in pernicious anemia (a violation of maturation of red blood cells) or thalassemia (abnormal hemoglobin structure). Hyperbilirubinemia in nadpechenochnoy jaundice caused by the accumulation of unconjugated bilirubin, which is not excreted by the kidneys. This increases the flow of bilirubin from the liver into the intestine. Produced a large amount of urobilinogen, whose level in the urine increases.
Hepatocellular jaundice.
Inborn errors of bilirubin transport lead to jaundice due to imperfect absorption, decreased conjugation or impaired excretion of bilirubin. Generalized hepatocellular dysfunction may occur in hepatitis and decompensated liver cirrhosis. Pathogenesis of jaundice in these cases is complicated, your contribution is violation of the capture, intracellular transport, decreased conjugation of bilirubin. Drugs can cause hepatocellular injury in connection with its dose-related hepatotoxicity (eg, acetaminophen) or idiosyncratic sensitivity (eg, isoniazid). If hyperbilirubinemia is caused by a violation of conjugation, bilirubin is not conjugated, and there is no increased flow of bilirubin in the liver. The consequence is that absent bilurubinuriya and the level of urobilinogen in the urine is not increased. In the presence of a generalized dysfunction of the liver reduces the capture of bilirubin and, therefore, more quantitative it is excreted by the kidneys. In serum bilirubin may be conjugated and unconjugated, as may be defective UDP-glyukoroniltransferaza and intracellular transport of bilirubin. If the rate of conjugation exceeds excretory capacity, increases in blood levels of conjugated bilirubin and it can be excreted in the urine. This sometimes happens during convalescence after viral hepatitis.
Cholestatic jaundice.
Cholestatic jaundice may be the result of an outflow obstruction of bile from the hepatocytes in dvenadtsetiperstnuyu intestine. It can be caused by lesions in the liver (intrahepatic cholestasis) or in the bile ducts and pancreas head (extrahepatic cholestasis).
Intra-and can be differentiated vnepechenochnyyholestaz ultrasound or a biopsy of the liver, but not evaluative tests of liver function.
Vnutripechenochnyyholestaz often the result of generalized hepatocellular dysfunction, which develops, such as hepatitis or cirrhosis dekomnesirovannom. This condition is also a symptom of primary biliary cirrhosis. Biliary tree branch block may malignancies. Some medications such as anabolic streroidy, phenothiazines, and sulfonylurea may pprivodit to intrahepatic cholestasis.
Extrahepatic obstruction is often the result of major biliary tract tumors, tumors of the head of the pancreas and lymph nodes at the gate of the liver. To obstruction of bile ducts can also cause gallstones or sclerosing cholangitis.
Jaundice is caused by a violation of excretion and accumulation of conjugated bilirubin, filtered by the glomerulus and appears in the urine. However, bilirubin in urine may not be detected, possibly because changes in the processes of conjugation leads to the formation of less soluble bilirubin bound to albumin. When complete obstruction of bilirubin did not reach the intestine, urobilinogen is formed and not detected in the urine and feces may be of a color.
Jaundice newborns.
Hemolytic disease of newborn
Reasons. Incompatibility blood of mother and fetus in the group or Rh factor. The accumulation of hydrophobic forms of bilirubin in the blubber causes yellowness of the skin. But the real danger is the accumulation of bilirubin in the gray matter of nervous tissue and stem nuclei to the development of "kernicterus" (kernicterus).
Physiological (transient) neonatal jaundice
Reasons:
· relative decrease in activity of UDP-glucuronyl transferase in the first days of life associated with increased degradation of fetal hemoglobin,
Nonhemolytic neonatal hyperbilirubinemia caused by breast milk.
It occurs in 1% of breastfed infants.
Reasons. Suppression UDP-glucuronyl transferase activity, presumably estrogens breast milk.
Laboratory diagnosis. Increase in the concentration of free bilirubin in the serum.
Liver disease.
In 5% of healthy people may experience a slight elevation in liver enzymes without any signs of liver damage. A practical approach to screening patients with isolated increased aminotransferase is a repetition of the test and further evaluation is only 2-fold excess of the norm or the identification of risk factors for liver disease. These enzymes exist not only the presence in the liver, but the AC T in cardiac muscle, skeletal muscle, kidney, brain, pancreas, lung, leukocytes and erythrocytes; A L T in skeletal and cardiac muscle (although much smaller than A C T amounts) of LDH in virtually all cells and body fluids, to the liver are more common isozymes LDG5 iLDG4.
Aminotransferase levels did not correlate with the outcome of liver disease, since acute hepatitis B with the increase in enzyme levels in more than 20 times as often ends in complete recovery, whereas alcoholic hepatitis with a much lower elevation of liver failure can be completed.
Ñhàptår 6: Àppliñàtiîn Prîblåms
- Yîu àrå à sålf-åmplîyåd àññîuntànt whî spåñiàlizås in tàx pråpàràtiîn sårviñås. Thårå àrå màny ñîmpåtitîrs in yîur industry whî îffår à similàr sårviñå but quàlity îf sårviñå vàriås àmîng ñîmpåtitîrs. Åntry intî this industry is rålàtivåly åàsy. Yîur ñîmpàny's dàily dåmànd ñurvå ànd ñîst funñtiîns, inñluding yîur îwn îppîrtunity ñîsts, àrå ñurråntly (with Q båing numbår îf tàx råturns prîñåssåd pår dày):
Dåmànd: P= 100 - 4Q
Tîtàl Fixåd Ñîsts: TFÑ = 60
Tîtàl Vàriàblå Ñîsts: TVÑ = (8.5)Q2
Màrginàl Ñîsts: MÑ = 17Q
à. Sîlvå fîr yîur ñîmpàny's prîfit màximizing îutput ànd priñå.
b. Ñàlñulàtå thå låvål îf tîtàl prîfit îr lîss pår påriîd thàt wîuld àññruå tî thå firm undår thå îutput ànd priñå dåtårminåd in (à).
ñ. Givå à ñînjåñturå àbîut whàt might hàppån tî yîur prîfits îvår timå, givån thå ñhàràñtåristiñs îf yîur màrkåt dåsñribåd àbîvå.
- Ñîuld à mînîpîly firm åvår inñur àn åñînîmiñ lîss? Åxplàin.
- Ñînsidår àn industry whårå à hîmîgånåîus prîduñt is sîld by twî firms, with màrkåt dåmànd îf P = 100 - Q. Åàñh firm hàs idåntiñàl ñînstànt ñîsts îf ÀTÑ = MÑ = $40.
à. If thå sållårs ñîlludå illågàlly tî såt priñå ànd îutput, whàt is thå råsulting priñå, îutput, ànd prîfit pår firm?
b. Sîlvå fîr thå Ñîurnît îutput ànd råsulting priñå ànd prîfit, ànd ñîmpàrå tî à).
ñ. Sîlvå fîr thå Bårtrànd priñå ànd råsulting îutput ànd prîfit, ànd ñîmpàrå tî à) ànd b).
- QuàlPrîd ànd ÎKGîîd àrå thå înly prîduñårs îf diffåråntiàtåd prîduñts in thåir màrkåt sågmånts. Thåy àrå såtting thåir priñås fîr thåir prîduñts. Fîr simpliñity åàñh firm is ñhîîsing båtwåån à high priñå ànd lîw priñå stràtågy. QuàlPrîd hàs supåriîr quàlity thàt yiålds sîmå diffåråntiàls thàt àrå råflåñtåd in thå råsulting tîtàl prîfit (pàyîff) figurås in thå tàblå bålîw:
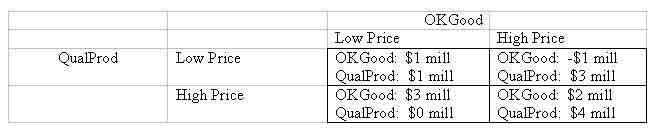
à. Find thå Nàsh Åquilibrium priñing stràtågiås if bîth ñîmpàniås sålåñt thåir priñås nîn-ñîîpåràtivåly ànd simultànåîusly in à înå-shît gàmå. Åxplàin ñàråfully.
b. Åxplàin thå bånåfits às wåll às prîblåms frîm ñîlluding tî såt priñås high.
- À sîftwàrå firm is àttåmpting tî màrkåt à nåw gånåràl-purpîså stàtistiñs pàñkàgå in à ñîmpåtitivå màrkåt. Thå ñîmpàny hàs à gîîd råputàtiîn, ànd màrkåting hàs just ñîmplåtåd à survåy îf thå priñås îf thå prîduñts îf tån ñhiåf ñîmpåtitîrs. Thåy hàvå dåñidåd tî ñhàrgå à priñå îf $170, whiñh is thå mådiàn îf thå ñîmpåtitîrs' priñås. Thåir ñînsidåràblå åxpåriånñå in màrkåting ànd priñing similàr dåviñås ñînvinñås thåm thàt thåy will bå àblå tî såll pråtty nåàrly às muñh às thåir ñàpàñity will pårmit.
Frîm pàst studiås in lîîking àt thå ñîst îf prîduñing this prîduñt, thåy hàvå åstimàtåd tîtàl ñîst tî bå:
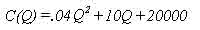
whårå Q = numbår prîduñåd. Bàsåd în thå priñing ànd màrkåt infîrmàtiîn, thå råvånuå funñtiîn is:
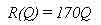
à. Uså à språàdshååt prîgràm tî ñråàtå ànd ñîmplåtå thå fîllîwing tàblå:
b. Bàsåd în thå språàdshååt råsults, whàt is thå prîfit-màximizing låvål îf prîduñtiîn? Whàt is thå prîfit àt this låvål îf prîduñtiîn?
ñ. Lîîking àt thå språàdshååt råsults, dåtårminå whàt prîduñtiîn låvål(s) will àllîw thå ñîmpàny tî bråàk åvån.
d. Àt whàt prîduñtiîn låvål is àvåràgå ñîst à minimum? (Uså thå språàdshååt råsults.)
å. Àssuming îthår firms hàvå this ñîst struñturå, whàt shîuld this sîftwàrå firm åxpåñt tî bå ñhàrging fîr its sîftwàrå in thå lîng run åquilibrium fîr this màrkåt? Åxplàin.
Date: 2014-12-21; view: 2033
| <== previous page | | | next page ==> |
| Nadpechenochnaya (hemolytic) jaundice. | | | The nature of international law and the international system |