
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Intraoperative angiography
With the proximal clamp in position a 5 or 8French baby-feeding catheter is inserted into the arteriotomy. The tip of the catheter is placed 5cm into the superficial femoral artery and distal control around it is achieved with a vessel-loop. Contrast for intravasal use containing 140–300 mg iodine/ml is infused with a 20ccsyringe connected to a three-way valve. Heparinized Ringer’s or saline (10units/ml heparin) is flushed through the catheter before and after contrast injection to prevent thrombosis in the occluded vascular bed. If the patient is suspected to have renal failure, the amount of contrast used is kept at a minimum. Angled projections can be obtained without moving the C-arm by rotating the patient’s foot.
The use of contrast in the Fogarty catheter balloon during fluoroscopy allows the calf vessel into which the catheter slides to be identified. The technique for intraoperative angiography is also a prerequisite for interoperative use of endovascular treatment options such asangioplasty (Fig. 9).
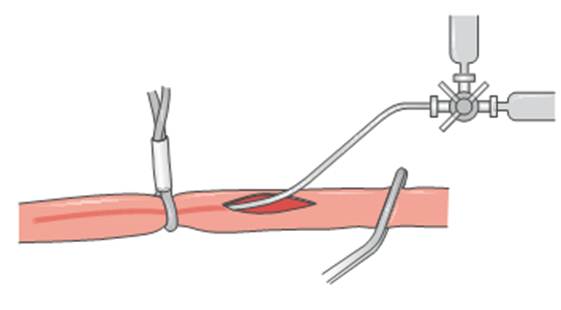
Fig. 9. Intraoperative angiography
Thrombolysis
Thrombolysis is performed in the angiosuite. A consultation with a specialist in coagulation disorders or a specialist in vascular medicine is sometimes needed to discuss possible problems related to coagulation before the procedure.
Treatment is usually directed toward resolving a fresh, thrombotic occlusion, but emboli and thrombi several weeks old can also be successfully lysed. The procedure starts with a diagnostic angiography via contralateral or antegrade ipsilateral arterial punctures. If thrombolytic treatment is decided the procedure continues right away, and the tip of a pulse-spray catheter is placed in the thrombus. The lytic agent is then forcefully injected directly into it to cause fragmentation. The primary choices for lytic agent are recombinant tissue plasminogen activator (rtPA) or urokinase. Because of the risk of allergic reactions, streptokinase should be avoided. Intermittent injections of 1 ml every 5–10 min to a total dose of 10–20 ml rtPA over 1–3 h is followed by angiographic control of the result. If the thrombus is completely lysed any underlying lesion is treated. If thrombus still remains, the rtPA infusion is continued slowly over 6–12h with 1mg/h. If the initial thrombolysis fails, a variety of mechanical catheters can be used to try to further dissolve and aspirate the thrombus. Examples include the AngioJet and the Amplatz.
Because of the risk of bleeding and systemic complications, and also because the ischemic leg may deteriorate, careful monitoring during con-tinued thrombolysis is necessary. This is best done in an intensive care or step-down unit. The patient should be kept supine in bed throughout the procedure. During this time the other measures suggested for optimizing coagulation and central circulation are continued. It is also necessary to check fibrinogen concentration to make sure the value does not decline to <1.0 mg/ml. Below this level surgical hemostasis is insufficient and the infusion should be stopped. Angiographic control of the result is performed afterwards, usually the following morning, and occasionally during the slow infusion to check the effect and allow repositioning of the catheter. The part of the thrombus surrounding the catheter is lysed first, which is why it often is beneficial to advance the catheter further into the thrombus after a few hours.
Finally, the lesion that caused the thrombosis is treated with angioplasty. To avoid unnecessary bleeding from the puncture site, the fibrinogen concentration is checked again before the sheath is withdrawn to ensure that the level exceeds 1.0 mg/ml.
Date: 2014-12-29; view: 1762
| <== previous page | | | next page ==> |
| TECHNICAL TIPS | | | Reperfusion Syndrome |