
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Operation
Exposure of Different Vessel Segments in the Leg
Femoral Artery in the Groin, Fig. 4 A, B, C.
a A longitudinal skin incision starting 1–2 cm cranial to the inguinal skin fold and continued lateral to the artery is used to avoid the inguinal lymph nodes. A common mistake is to place the incision too far caudally, which usually means the dissection is taking place distal to the deep femoral.
b The dissection is continued sharply with the knife straight down to the fascia lateral to the lymph nodes and is then angulated 90° medially to reach the area over the artery. It should then be palpable. Lymph nodes should be avoided to minimize the risk for infection and development of seroma. The fascia is incised, and the anterior and lateral surfaces of the artery are approached.
c At this stage the anatomy is often unclear regarding the relation of branches to the common femoralartery. Encircle the exposed artery with a vessel-loop, and gently lift the artery. Continue dissection until the bifurcation into superficial and deep femoral artery is identified. Its location varies from high up under the inguinal ligament up to 10 cm further down. At this stage, the surgeon must decide whether exposure and clamping of the common femoral are enough. This is usually the case for proximal control in trauma distally in the leg. In acute ischemia it is more common that the entire bifurcation needs to be exposed.
During the continued dissection, attention must be given to important branches that should be controlled and protected from iatrogenic injuries. These are, in particular, the circumflex iliac artery on the dorsal aspect of the common femoral artery and the deep femoral vein crossing over the anterior aspect of the deep femoral artery just after its bifurcation. To provide a safe and good exposure of the deep femoral to a level below its first bifurcation, this vein must be divided and suture-ligated. Partial division of the inguinal ligament is occasionally needed for satisfactory exposure.
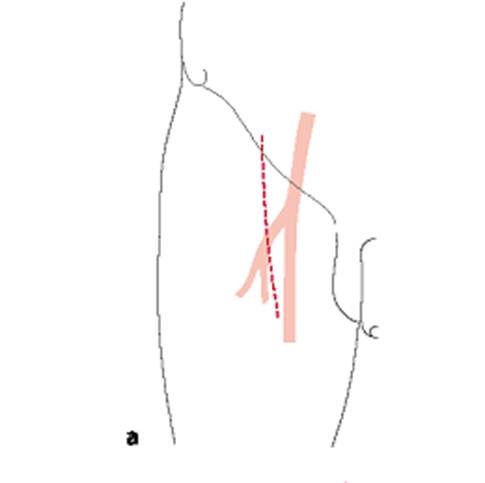
Fig. 4 A. Exposure of femoral artery in the groin
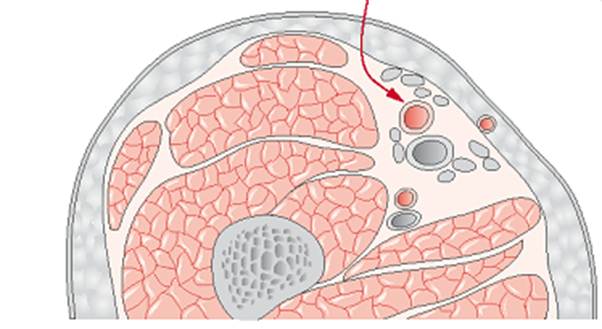
Fig. 4 B. Exposure of femoral artery in the groin
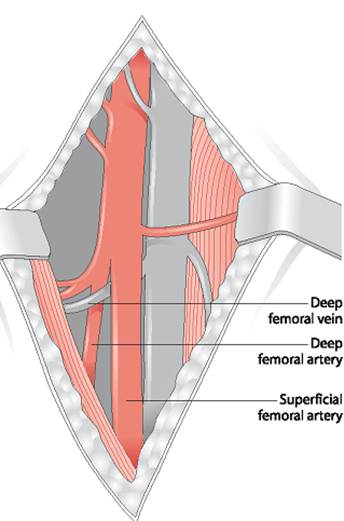
Fig. 4 C. Exposure of femoral artery in the groin
Superficial Femoral Artery, Fig. 5
A skin incision is made along the dorsal aspect of the sartorius muscle at a midthigh level. It is important to avoid injuries to the greater saphenous vein, which usually is located in the posterior flap of the incision. The incision can be elongated as needed. After the deep fascia is opened and the sartorius muscle is retracted anteriorly, the femoral artery is found and can be mobilized. Division of the adductor tendon is sometimes required for exposure.
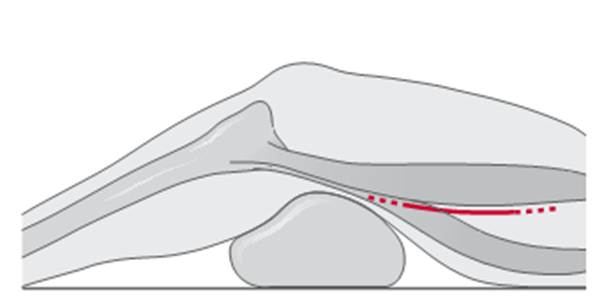
Fig. 5. Incision for exposure of the supericial femoral artery
Popliteal Artery Above the Knee, Fig. 6 A, B.
a The knee is supported on a sterile, draped pillow. The skin incision is started at the medial aspect of the femoral condyle and follows the anterior border of the sartorius muscle 10–15 cm in a proximal direction. Protect the greater saphenous vein and the saphenous nerve during dissection down to the fascia. After dividing the fascia longitudinally, continue the dissection in the groove between the sartorius and gracilis muscles, which leads to the fat in the popliteal fossa.
b The popliteal artery and adjacent veins and nerve are then, without further division of muscles, easily found and separated in the anterior aspect of the fossa.

Fig. 6 A. Exposure of popliteal artery above the knee

Fig. 6 B. Exposure of popliteal artery above the knee
Popliteal Artery Below the Knee, Fig. 7 A,B.
a A sterile pillow or pad is placed under the distal femur. The incision is placed 1 or 2 cm posterior to the medial border of the tibia, starting at the tibial tuberosity and extending 10–12 cm distally. Subcutaneous fat and fascia are sharply divided, with caution to the greater saphenous vein.
b The popliteal fossa is reached by retracting the gastrocnemius muscle dorsally. The deep fascia is divided and the artery usually easier to identifiy. Occasionally, pes anserinus must be divided for adequate exposure. The popliteal artery is often located just anterior to the nerve and in close contact with the popliteal vein and crossing branches from concomitant veins. If it is necessary to expose the more distal parts of the popliteal artery, the soleus muscle has to be divided and partly separated from the posterior border of the tibia.
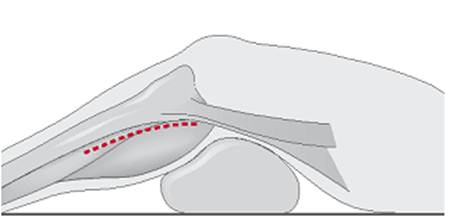
Fig. 7 A. Exposure of popliteal artery below the knee
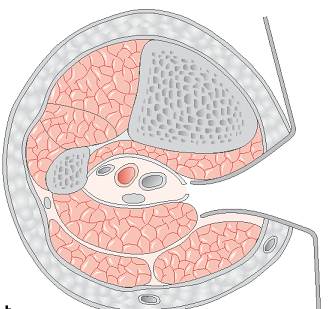
Fig. 7 B. Exposure of popliteal artery below the knee
Embolectomy
It is beyond the scope of this book to cover the technique for vascular reconstructions. But because embolectomy from the groin with balloon catheters (known as Fogarty catheters) is one of the most common emergency vascular operations in a general surgical clinic and may be performed by surgeons not so familiar with vascular surgery.
Date: 2014-12-29; view: 2508
| <== previous page | | | next page ==> |
| Management and Treatment | | | TECHNICAL TIPS |