
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
ACUTE LEG ISCHEMIA
Acute leg ischemia is associated with a great risk for amputation and death. The age of the patients is high, and to some extent acute leg ischemia can be considered an end-of-life disease. Patients’ symptoms and the clinical signs of the afflicted leg vary. Sometimes grave ischemia immediately threatens limb viability, such as after a large embolization to a healthy vascular bed. Other times the symptoms are less dramatic, appearing as onset of rest pain in a patient with claudication. This is usually due to thrombosis of a previously stenosed artery.
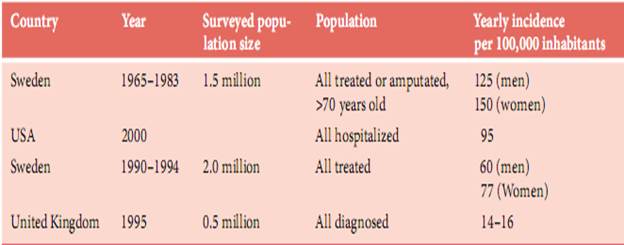
Table 2.Incidence of acute leg ischemia
It is the severity of ischemia that determines management and treatment. To minimize the risk for amputation or persistent dysfunction it is important to rapidly restore perfusion if an extremity is immediately threatened. When the leg shows signs of severe ischemia but is clearly viable, it is equally important to thoroughly evaluate and optimize the patient before any intervention is initiated. These basic management principles are generally applicable. Accordingly, we recommend “management by severity” rather than “management by etiology” (thrombosis versus embolus) but recognize that the latter can also be an effective strategy.
Embolism
Embolism is by far the most common cause of acute arm ischaemia, accounting for 74–100% of cases.
In the lower extremities, controversy exists regarding the ratio between arterial embolism and thrombosis, with diferent studies giving numbers ranging from 4:1 to 1:9.
The heart is invariably the most common origin of peripheral arterial emboli, and is responsible for 58–93% of cases. However, the pattern of the underlying heart disease has changed recently as the incidence of rheumatic valvular disease has decreased significantly
Cardiac Sources of Emboli
Nowadays, the most common sources of arterial emboli of cardiac origin are:
atrial ibrillation due to atherosclerotic heart disease, accounting for 32–75% of cases, followed by
myocardial infarction with mural thrombi formation, which is responsible for 21–32% of peripheral emboli.
Less common cardiac sources of emboli are:
idiopathic dilated cardiomyopathy
prosthetic valves
rheumatic mitral valve disease
intracavitary cardiac tumours (mainly myxomas)
paradoxical embolization through an intracardiac defect, usually a patent foramen ovale
fungal or bacterial endocarditis.
Date: 2014-12-29; view: 1232
| <== previous page | | | next page ==> |
| Operation | | | Thrombosis |