
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Physiopathology of main symptoms and their clinical display
From the pathogenetic point of view the primary significance in the development of clinical symptomatology belongs to an increase of the volume of tumour, that results in the direct and mediated development of the syndrome of the increased intracranial pressure and the whole range of focal symptomatology.
The formation of the hypertensive syndrome takes place for three reasons. First, the growth of the tumour focus leads to the increase of the volume of the tissue component in the cranial cavity. Second, in a certain location of tumour, disturbance of outflow of liquor is possible, that results in the increase of its volume in the cavities of the ventricular system. And, finally, third, an expansive growth of tumour in certain cases can cause compression of the surrounding cerebral tissue, including vessels of different caliber, that determines its ischemization, a decrease of production of ATP, the disturbance of work of ATP-dependent ionic interchanges which provide the maintenance of the normal balance of ions between tissue compartments (intracellular medium, intercellular space, vascular bloodstream). The latter is accompanied by the increase of the osmolality of the extravascular medium and the accumulation of water in the ischemizied foci of brain tissue. The swiftness of the development of edema-swelling of cerebral tissue initiated on the periphery of the tumour node can be the main factor of further spreading of this process and involving of still vaster areas of the brain.
Compression of the areas of the brain immediately adjacent to the tumour focus results in the development of focal symptomatology. The compression of areas of brain tissue located at some distance from the tumour focus under the action of the spreading process of edema-swelling, ischemia or because of the growth of tumour results in the appearance of symptomatology at a distance. In the most advanced case the conditions appear for the dislocation of cerebral tissue and formation of symptoms of dislocation syndrome.
A local compression of brain tissue or an increase of intracranial pressure and irritation of receptors of arachnoid membranes become possible as a sequence of the constancy of the volume of the cranial cavity. In compliance with Monroe- Kelly's doctrine, a change of the volume of one of three components of the content of the cranial cavity (tissue, blood, liquor), takes place due to the diminishing of the volume of two remaining ones. The growth of tumour above all things results in a local diminishing of the blood flow and is accompanied by the diminishing of the volume of liquor in the cranial cavity. The increase of the volume of blood in the cavity of the skull has considerable consequences, as a rule, aggravating a perfusion situation in brain tissue. Taking into account the mechanism of the development of edema-swelling of the brain, one can see that the state of compensation will be sooner or later disturbed, and that will result in the appearance of a vicious circle: "ischemia - edema - an increase of tissue pressure - ischemia".
The described nosotropic features of the development of tumour process explain, one the side, the possibility of a long-term growth of tumour in functionally inert areas of the brain in the absence of apparent symptomatology, and, from the other side, the presence of brain tumours which even at small sizes and a limited period of growth give an apparent clinical symptomatology.
In a clinical respect, they distinguish general cerebral and focal symptomatology arising in connection with the development of brain tumour.
The most significant and one of the earliest symptoms of the development of intracranial hypertension because of the growth of tumour is headache. This symptom is observed in 92% of patients with subtentorial and in 77% with supratentorial tumours and arises due to the tension and compression of the dura mater of the brain. At the beginning of the disease a headache is most frequently of a diffuse nature, being dull, inconstant, bursting open. With the increase of the intracranial pressure, the pain increases acquiring a permanent character. A characteristic but not a constant feature of the headache arising because of the development of intracranial hypertension, is its appearance or strengthening in the second half of night, at down, that is related to the increase of the liquor pressure in this period of day. Sometimes against the background of a permanent headache there arises its attack-like strengthening which is accompanied by vomiting, dizziness, a decrease of the level of consciousness.
As a typical for brain tumours one should consider the appearance or strengthening of headache at agitation, exercise stress. To the rank of classic they refer the connection of the intensity of the pain feelings with the position of the head of the patient in tumours of IVth ventricle: the pain subsides in the position of the patient on the side of the localization of tumour (Bruns's symptom), that is explained by the gravity displacement of the tumour node. At the same time, in elderly people even in the presence of tumour of large sizes pain symptomatology can be for a long time absent. In benign neoplasms of arachnoid membranes the pain is of a local nature, sometimes irradiates to specific areas and at the superficial location of the tumour node can be accompanied by a local painfulness at percussion. However, such variants of pain symptomatology are of less importance in making a preliminary diagnosis.
Vomiting occurs in 68% of patients with brain tumours. Most frequently, this symptom is related to the development of intracranial hypertnesion but sometimes can the conditioned by the presence of tumour of IVth ventricle or of the cerebellum which produces a direct mechanical effect on the vomiting center. A classic characteristic of the so-called tumorous vomiting is its appearance in the morning, without preliminary nausea, on an empty stomach and at the peak of headache . After vomiting, the intensity of the headache diminishes that is related to the coming dehydrating effect and the decrease of the intracranial pressure. The frequency of vomiting is variable.
A frequent neuroophthalmologic symptom which reflects the presence of intracranial hypertension is stagnant disks of optic nerves. In most cases, this symptom comes to light simultaneously from both sides, but sometimes its appearance can differ in time. The speed of the development of this symptom depends on the speed of the growth of intracranial hypertension. The stagnation of disks of visual nerves is most frequently determined in a complex with other hypertensive symptoms. And only in certain cases (e.g. in children) the symptom can take a debut character.
The increase of intracranial pressure results in disturbances of the activity of peripheral parts of the visual analyzer, that is related above all things to the swelling of tissue of the optic nerve and the retina of an eye. Subjectively the patients notes a periodic appearance of shroud in front of the eyes, "flies" in early hours. A long- term increase of intracranial pressure results in the development of the secondary atrophy of optic nerves. At that, the decrease of visual acuity arising because of the development of atrophy is irreversible. Carrying out radical operative intervention or long-term normalization of intracranial pressure do not often result in compromising the progression of the loss of sight. In case of the development of tumour process in the anterior or middle cranial fossa with the compression of the optic nerve on the side of tumour one observes quite often Foster-Kennedy's symptom of a combination of the primary atrophy of the optic nerve on the side of the growth of tumour with the secondary atrophy of an opposite optic nerve because of the development of the hypertensive syndrome.
Dizziness is observed as a general cerebral symptom in intracranial hypertension in 40-50% of patients with brain tumours. The appearance of this symptom is related to the development of the stagnant phenomena in the vestibular labyrinth and increase of pressure of the endolymph in the semicircular ducts. In some cases, it can become apparent as an element of focal symptomatology in tumours of the cerebellum, VIII nerve, pons and IV ventricle. The displays of the symptom are described by patients as the sense of rotation of surrounding objects and one's own body, the feeling of collapsing. Dizzinesses, arising as a result of intracranial hypertension become apparent at later stages of the development of the pathological process. In any case, this symptom arises, as a rule, as an attack-like, quite often after a considerable increase of the intracranial pressure. Often dizziness is accompanied by nausea, vomiting, sonitus, vegetative disorders and even a decrease of the clarity of consciousness.
Disorders of psyche in the context of the development of general symptomatology occur in 63-78% of patients. As the main nosotropic moments in the development of such a type of disorders one should regard the disorder of the perfusion by the blood of the brain tissue, especially its truncal parts, that is a direct consequence of the growth of intracranial pressure, intoxication of the brain by the products of disintegration and factors which are produced in the tumour focus, as well as the diffuse dysfunction and disturbance of the anatomic integrity of the associative pathways of the brain. It is also necessary to note that psychical disorders are elements of focal symptomatology in tumours of the frontal area of the head. In this case, the development of disorders of the patient's psyche takes place under the effect of both general cerebral and local pathogenetic mechanisms.
The nature of psychical disorders arising brain tumours, can be different. Thus, against the background of clear consciousness, the appearance of derangements of memory, thinking, perception, capacity of concentration is possible. In certain cases, aggressiveness, inclination to an amotivational behavior, displays of negativism, a decrease of criticism are brought to the forefront. Sometimes such a clinical picture can be shifted by the phase of apathy, languor. In certain cases, there is the development of delirium and gallucinations.
In elderly patients the development of psychical disorders is practically always accompanied by an increase of intracranial pressure and quite often is the earliest clinical sign, especially in the presence of hypertensive disease and atherosclerosis.
The level of consciousness is the main clinical equivalent of the perfusion of the brain by blood and intracranial pressure. Therefore, the progress of intracranial hypertension inevitably results in the gradual suppressing of consciousness which without carrying out adequate medical measures passes to the state of sopor and coma.
To the rank of general cerebral symptoms and symptomocomplexes it is also necessary to refer to a certain extent the development of the epileptic syndrome. After different data, the arising of this syndrome is observed in 22-30,2% of patients with brain tumours, as a rule, of supratentorial localization. More frequent episyndrome accompanies the development of astrocytic tumours, rarer - meningiomas. In 37% of patients, epiattacks are the debut symptom of brain growth. Therefore, their appearance without obvious reasons at the age over 20 years must be regarded above all things from the point of view of oncologic suspicion. As well as in the case of psychical disorders, in the development of the episyndrome not only of general cerebral pathogenetic mechanisms but also local (focal) effects of tumour on brain tissue. It is of particular importance in the analysis of reasons of the development of tumours of the temporal lobe and closely located areas of the brain. In this case the formation of the epileptic focus of an increased excitability of nervous cells (for example, in the associative areas of the temporal lobe) takes place in the context of the development of focal "in the neighbourhood" symptomatology. A local component in formation of the epileptic syndrome is also determined by the nature of the aura anticipating an attack. For example, the so-called motor auras are observed in the development of the epileptic syndrome in tumours of the frontal lobe, sensitive hallucinations -in tumours of the parietal lobe, olfactory, auditory and complicated visual - in tumours of the temporal lobe, simple visual - in tumours of the cervical lobe.
The nature of epileptic attacks arising in the development of brain tumour varies from small attacks (petit mal) to the generalized convulsive attacks (grand mal). An important sign allowing to bind an epileptic attack to the development of tumour process is postattack prolapse of function of the motor or speech sphere.
Focal symptomatology arises because of a local direct or mediated effect of tumour on brain tissue and reflects the disorder of its certain parts (or separate craniocerebral nerves). They distinguish primary (direct) focal symptoms which reflect the result of the action of tumour on the immediately adjacent areas of the brain, as well as secondary focal symptoms, in the development of which a leading role is played by not so much direct mechanical influence of tumour, as by ischemia and edema-swelling of the surrounding cerebral tissue . Depending on the degree of remoteness of the focus of secondary symptomatology from the tumour node, it is accustomed to distinguish the so-called "in the neighbourhood" and "at a distance" symptoms.
Mechanisms of the development of focal symptomatology are different. Thus, primary focal symptoms arise due to the direct mechanical and chemical effect of the tumour focus on the adjacent brain tissue and its ischemization. The degree of the apparency and duration of such an influence determine the nature of primary focal symptomatology: first, the symptoms of irritation or hyperfunction of the indicated area of brain tissue become apparent which are subsequently substituted for the symptoms of prolapse.
To the symptoms of irritation they refer jacksonian epilepsy and Kojewnikoff s epilepsy, shaped and shapeless hallucinations, epileptic equivalents, auras. To the symptoms of prolapse they refer pareses, paralyses, defects of visual fields, aphasias, anesthesia’s.
The appearance of "in the neighbourgood" symptoms is related to ischemia of the corresponding areas of the brain because of primary compression, as well as due to the mechanical effect of tumour on the main vessels supplying with blood the corresponding areas of the brain (e.g. truncal symptoms in tumours of the cerebellum, motor aphasia in tumors of the pole of the left frontal lobe, damage of nerves of IIId and IVth pair in tumours of the temporal lobe.
"At a distance" symptoms arise only in case of an advanced process and in the progress of general cerebral symptomatology can grow into dislocation syndromes. The examples of "at a distance" symptoms is verbal hallucinosis in tumours of the posterior cranial fossa, symptomocomplexes rising in the compression of certain areas of the brain as dislocations.
In the dislocation of brain tissue there can arise its incarceration in anatomic apertures inside the skull or at the outlet out of it. Such a situation is denoted by the term "dislocation syndrome" of a certain area of the brain (Fig. 1).
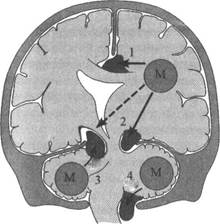
Fig. 1. Mechanism of formation of different types of dislocations in brain tumours (M): 1-semilunar dislocation; 2-temporal-tentorial dislocation; 3-cerebellotentorial dislocation; 4-dislocation of tonsils of the cerebellum into the cervicodural funnel
Date: 2015-02-16; view: 1327
| <== previous page | | | next page ==> |
| Classification of brain tumours | | | The main variants of dislocations |