
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Dynamics of Addiction
Drug addiction is a chronically relapsing disorder characterized by compulsive drug use and loss of control over drug intake. Addiction comprises three stages: preoccupation/anticipation, binge/intoxication, and withdrawal/negative affect, in which impulsivity often dominates at the early stages, and compulsivity dominates at terminal stages. As an individual moves from impulsivity to compulsivity, a shift occurs from positive reinforcement driving the motivated behavior to negative reinforcement driving the motivated behavior (Koob, 2004). These three stages are conceptualized as feeding into one other, becoming more intense, and ultimately leading to the pathological state known as addiction (Koob and Le Moal, 1997). The preoccupation/anticipation (craving) stage of the addiction cycle has long been hypothesized to be a key element of relapse in humans and defines addiction as a chronic relapsing disorder (Tables 1 and and22).

Table 1
Definitions
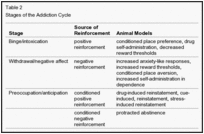
Table 2
Stages of the Addiction Cycle
Different drugs produce different patterns of addiction that engage different components of the addiction cycle, depending on dose, length of use, and even cultural factors. With opioids, the classic drugs of addiction, a pattern of compulsive intravenous or smoked drug taking evolves that includes intense intoxication, the development of tolerance, escalation in intake, and profound dysphoria, physical discomfort, and somatic and emotional withdrawal signs during abstinence. A pattern develops in which the drug must be obtained to avoid the severe dysphoria and discomfort experienced during abstinence. Alcohol addiction or alcoholism can follow a similar trajectory, but the pattern of oral drug taking often is characterized by binges of alcohol intake that can be daily episodes or prolonged days of heavy drinking and is characterized by a severe somatic and emotional withdrawal syndrome. Nicotine addiction contrasts with the above patterns, with little obvious signs of the binge/intoxication stage, and has a pattern of intake characterized by highly titrated intake of the drug except during periods of sleep and negative emotional states during abstinence, including dysphoria, irritability, and intense craving. Marijuana addiction follows a pattern similar to opioids and tobacco, with a significant intoxication stage, but as chronic use continues, subjects begin to show a pattern of use characterized by chronic intoxication during waking hours followed by a withdrawal that includes dysphoria, irritability, and sleep disturbances. Psychostimulant addiction (cocaine and amphetamines) shows a pattern with a salient binge/intoxication stage. Such binges can be hours or days in duration and often are followed by a withdrawal (?crash?) characterized by extreme dysphoria and inactivity. Intense craving for all drugs can anticipate withdrawal (i.e., with opioids, alcohol, nicotine) or often occurs after acute withdrawal when craving is driven by both environmental cues signifying the availability of the drug and internal states linked to negative emotional states and stress.
Animal models of the symptoms of addiction on specific drugs such as stimulants, opioids, alcohol, nicotine, and Δ9-tetrahydrocannabinol can be defined by models relevant to different stages of the addiction cycle (Shippenberg and Koob, 2002) (Table 2). Animal models for the binge/intoxication stage of the addiction cycle can be conceptualized as measuring acute drug reward, in which reward can be defined as a positive reinforcer with some additional emotional value, such as pleasure (Table 1). Animal models of reward and reinforcement are extensive and well validated and include intravenous drug self-administration, conditioned place preference, and decreased brain reward thresholds. Animal models of the withdrawal/negative affect stage include conditioned place aversion (rather than preference) to precipitated withdrawal or spontaneous withdrawal from chronic administration of a drug, increases in brain reward thresholds, and dependence-induced increases in drug seeking (Table 2). Rodents will increase intravenous or oral self-administration of drugs with extended access to the drugs and during withdrawal from the dependent state, measured both by increased drug administration and increased work to obtain the drug. Such increased self-administration in dependent animals has been observed with cocaine, methamphetamine, nicotine, heroin, and alcohol (Ahmed et al., 2000; Ahmed and Koob, 1998; Kitamura et al., 2006; O?Dell and Koob, 2007; Roberts et al., 2000). This model will be a key element for the evaluation of the role of brain stress systems in addiction outlined below.
Animal models of craving (preoccupation/anticipation stage) involve reinstatement of drug seeking following extinction from the drugs themselves, by cues linked to the drug, and from exposure to stressors (Shaham et al., 2003) (Table 1). Drug-induced reinstatement first involves extinction and then a priming injection of the drug. Latency to reinitiate responding or the amount of responding on the previously extinguished lever are hypothesized to reflect the motivation for drug-seeking behavior. Similarly, drug-paired or drug-associated stimuli can reinitiate drug-seeking behavior (cue-induced reinstatement). Stress-induced reinstatement involves the application of acute stressors that reinitiate drug-seeking behavior in animals that have been extinguished from the drug. These stressors can include physical stressors such as footshock, psychological stressors such as restraint, or pharmacological stressors such as yohimbine (Shaham et al., 2003). In rats with a history of dependence, protracted abstinence can be defined as a period after acute physical withdrawal has disappeared in which elevations in ethanol intake over baseline and increased stress responsivity persist (e.g., 2?8 weeks postwithdrawal from chronic ethanol). Protracted abstinence has been linked to increased brain reward thresholds and increases in sensitivity to anxiety-like behavior that have been shown to persist after acute withdrawal in animals with a history of dependence. Stress-induced reinstatement of drug seeking and stress-induced reinstatement of anxiety-like states during protracted abstinence will be used in the present review to explore the role of the brain stress systems in the preoccupation-anticipation (craving) stage of the addiction cycle (Table 2).
The thesis of this review is that a key element of the addiction process involves a profound interaction with brain stress systems and dysregulation of brain antistress systems to produce the negative emotional state that becomes the powerful motivation for drug seeking associated with compulsive use in the withdrawal/negative affect and preoccupation/anticipation (craving) stages of the addiction cycle. Chronic use of drugs of abuse has long been associated with exaggerated responses to stressors, and these exaggerated responses contribute to addiction (Himmelsbach, 1941). Delineation of key elements of not only hormonal but also brain stress neurocircuits have laid the foundation for new insights into the pathophysiology of addiction.
Date: 2016-06-12; view: 478
| <== previous page | | | next page ==> |
| FUTURE RESEARCH DIRECTIONS | | | Effects of Drug Withdrawal on CRF Levels in the Amygdala |