
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
TABLE XI-68 Diagnostic Criteria for Chronic Fatigue Syndrome
Characterized by Persistent or Relapsing Unexplained Chronic Fatigue
Fatigue lasts for at least 6 months.
Fatigue is of new or definite onset.
Fatigue is not the result of an organic disease or of continuing exertion.
Fatigue is not alleviated by rest.
Fatigue results in a substantial reduction in previous occupational, educational, social, and personal
activities.
Four or more of the following symptoms are concurrently present for 6 months:
Impaired memory or concentration, sore throat, tender cervical or axillary lymph nodes, muscle pain, pain
in several joints, new headaches, unrefreshing sleep, or malaise after exertion.
Exclusion Criteria
Medical condition explaining fatigue
Major depressive disorder (psychotic features) or bipolar disorder
Schizophrenia, dementia, or delusional disorder
Anorexia nervosa, bulimia nervosa
Alcohol or substance abuse
Severe obesity (BMI >40)
XI-69. The answer is B.(Chap. 389) Cognitive behavioral therapy (CBT) and graded exercise therapy (GET) have been found to be the only beneficial interventions in chronic fatigue syndrome (CFS). CBT is a psychotherapeutic approach directed at changing condition-related cognitions and behaviors. CBT for CFS aims at changing a patient's perpetuating factors by exploiting various techniques and components. The intervention, which typically consists of 12-14 sessions spread over 6 months, helps CFS patients gain control over their symptoms. GET is based on the model of deconditioning and exercise intolerance and usually involves a home exercise program that continues for 3-5 months. Walking or cycling is systematically increased, with set target heart rates. Evidence that deconditioning is the basis for symptoms in CFS is lacking, however. The primary component of CBT and GET that results in a reduction in fatigue is a change in the patient's perception of fatigue and focus on symptoms. CBT is generally the more complex treatment, which might explain why CBT studies tend to yield better improvement rates than GET trials. Not all patients benefit from CBT or GET. Predictors of poor outcome are somatic comorbidity, current disability claims, and severe pain. CBT offered in an early stage of the illness reduces the burden of CFS for the patient as well as society in terms of decreased medical and disability-related costs. Full recovery from untreated CFS is rare: the median annual recovery rate is 5% (range 0-31%) and the improvement rate 39% (range 8-63%). Major depressive disorder, bipolar disorder, eating disorder, and schizophrenia are exclusion criteria for the diagnosis of chronic fatigue syndrome.
XI-70. The answer is D.(Chap. 391) This patient is experiencing her first episode of a panic attack and does not meet the criteria for panic disorder. In this situation, no specific treatment is required. The patient should be reassured in a manner that is empathetic and supportive that she does not have any evidence of a serious medical disorder. Panic attacks are common, with about 1-3% of the population experiencing at least one panic attack. Panic attacks begin abruptly, most commonly without an immediate precipitating cause, and peak in severity over 10 minutes. The symptoms usually subside
spontaneously over the course of an hour. Diagnostic criteria for a panic attack include a minimum of four of the following criteria: palpitations or racing heart, sweating, trembling, shortness of breath, feeling of choking, chest pain, nausea or GI distress, dizziness, derealization, fear of losing control, fear of dying, paresthesias, or chills/hot flushes. If a patient subsequently develops panic disorder, a variety of treatment options can be pursued. Panic disorder is marked by at least 1 month of recurrent panic attacks associated with excessive worry about or change in behavior as a result of the attacks. The goals of therapy for panic attacks are to decrease the frequency of attacks and the severity of symptoms during the attack. Antidepressant medications are the cornerstone of therapy with selective serotonin reuptake inhibitors being the most frequently used class of medication. The dose of medication for panic disorder is typically lower than the antidepressant dose. For fluoxetine, this would be 5-10 mg daily. As these medications take 2-6 weeks to become effective, they are often combined with benzodiazepines to be used on an as-needed basis for immediate relief of attacks. Alprazolam and clonazepam are common agents used for panic disorder, although alprazolam may have more associated dependence with the need for escalating doses of medications. In combination with pharmacologic therapy, psychotherapy and education are also useful for the treatment of panic disorder. The therapy often includes breathing techniques, cognitive behavioral therapy, and even homework assignments.
XI-71. The answer is A.(Chap. 391) There are increasing numbers of antidepressant medications available in a variety of classes. Selective serotonin reuptake inhibitors (SSRIs) are the most commonly used antidepressant drugs. This class of medications includes fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, and escitalopram. These medications are taken once daily and have side effects including sexual dysfunction, headache, and insomnia. Tricyclic antidepressants were commonly used in past decades for the treatment of depression. However, overdoses can be lethal, and anticholinergic side effects including dry mouth, constipation, and urinary retention can limit the dose. Medications in the tricyclic class of antidepressants include amitriptyline, nortriptyline, imipramine, desipramine, doxepin, and clomipramine. Mixed norepinephrine/serotonin reuptake inhibitors and receptor blockers are a newer class of medications. These medications are increasing in use as they are quite effective and do not have the same frequency of sexual dysfunction. Medications in this class include venlafaxine, desvenlafaxine, duloxetine, and mirtazapine. Monoamine oxidase inhibitors were once a common antidepressant class of medication, but these medications are now only rare used. There is a wide range of drug and food interactions that can lead to hypertensive crises. Examples of medication in this class include phenelzine, tranylcypromine, and isocarboxazid. A final class of antidepressants is called simply mixed action drugs and includes trazodone, bupropion, and nefazodone.
XI-72. The answer is E.(Chap. 391) Post-traumatic stress disorder (PTSD) was only added as a discrete disorder in 1980. The diagnostic criteria for PTSD are long and require that an individual experiences an event where there was an actual or perceived threat of death or serious injury and that the individual's reaction included intense fear or helplessness. Following the event, the individual continues to re-experience the event and avoids stimuli associated with the trauma. In association with this, there is also often a generalized withdrawal and decrease in responsiveness. At the same time, the patient exhibits an increase in arousal that is often exhibited by insomnia, irritability, hypervigilance, and difficulty concentrating. Treatment of PTSD is almost always multifactorial, including both pharmacotherapy and psychotherapy. It is not uncommon for an individual with PTSD to develop a dependence on drugs or alcohol as an attempt to control the symptoms, and any substance abuse issues
need to be treated simultaneously as well. This patient's treatment would include avoidance of alcohol and intensive substance abuse treatment as needed. Treatment with antidepressant medications can decrease anxiety and avoidance behaviors. Trazodone is often given at night for its sedating properties. Psychotherapeutic strategies include cognitive behavioral therapy to overcome avoidance behaviors as well.
XI-73. The answer is B.(Chap. 391) Fifteen percent of the population will experience at least one episode of major depression over the course of a lifetime, and most episodes of major depression are treated by primary care practitioners. Treatment can be any of a number of medications across a variety of classes. Despite the popularity of newer antidepressants, there is no evidence that these medications are more efficacious than older drugs like tricyclic antidepressants. Indeed, 60-70% of patients will respond to any drug chosen if given in a sufficient dose for 6-8 weeks. Once a patient has been on treatment for about 2 months, the response should be evaluated, and if there has been an insufficient response, a dosage increase should be considered. In this patient, a dosage increase yielded control of depressive symptoms at 4 months. Once control of symptoms has been achieved, the drug should be continued for an additional 6-9 months to prevent relapse. If a patient experiences any additional episodes of major depression, he or she will likely require indefinite maintenance treatment.
XI-74. The answer is A.(Chap. 392) Alcohol is primarily absorbed through the proximal small intestine, but small to moderate amounts can also be absorbed in the mouth, esophagus, stomach, and large intestines. Several factors can increase the rate of absorption. One factor that increases absorption is rapid gastric emptying, which can be induced by concurrent consumption of carbonated beverages. Another factor that increases absorption from the gut to the blood is the ingestion of alcohol in the absence of other calorie sources such as proteins, fat, or carbohydrates. A final factor that can increase absorption is to drink alcohol that is diluted to a modest concentration (-20% or less). At high alcohol concentrations absorption is decreased, although high blood levels may be achieved because the amount of alcohol ingested is high.
XI-75. The answer is C.(Chap. 392) Alcohol has effects on many neurotransmitters in the brain. The predominant effect of alcohol lies in its ability to cause the release of y-aminobutyric acid (GABA) and acts primarily at the GABAA receptors. GABA is the primary inhibitory neurotransmitter in the brain
and is associated with the sedative effects of alcohol. Many other drugs affect the GABA system including benzodiazepines, nonbenzodiazepine sleep aids such as zolpidem, anticonvulsants, and muscle relaxants. The euphoric effects of alcohol consumption are related to increases in dopamine, which is common to all pleasurable activities. The effects on dopamine are thought to be important in alcohol craving and relapse. In addition, alcohol alters opioid receptors and can lead to a release of beta endorphins during acute ingestion. In addition to these effects, alcohol also inhibits postsynaptic N-methyl-D-aspartate excitatory glutamate receptors. Glutamate is the primary excitatory neurotransmitter of the brain, and its inhibition further contributes to the sedative effects of alcohol. Additional important effects on neurotransmitters include increased serotonin activity and decreased nicotinic acetylcholine receptors.
XI-76. The answer is D.(Chap. 392) The acute effects of any drug depend on many factors including amount consumed and absorbed, presence of other drugs, and past experience with the drug. In an individual who is naive to alcohol, drug levels as low as 0.02 g/dL can lead to a decrease in inhibitions
and a slight feeling of intoxication. In the United States, "legal" intoxication occurs at a blood alcohol level of 0.08 g/dL in most states. At this level, decreases in cognitive and motor abilities are seen. Once an alcohol level of 0.20 g/dL is achieved, an individual is obviously impaired with slurred speech, poor judgment, and impaired coordination. Light coma and depression of respiratory rate, blood pressure, and pulse occur at levels of around 0.30 g/dL, and death is likely to occur at levels of 0.40 g/dL. However, in individuals who drink heavily, tolerance begins to develop to alcohol. After a period of 1-2 weeks of daily alcohol consumption, liver metabolism of alcohol increases by as much as 30%, but disappears quite quickly with abstinence. Cellular or pharmacodynamic tolerance also occurs and refers to the neurochemical changes that allow an individual to maintain more normal physiologic functioning despite the presence of alcohol.
XI-77. The answer is C.(Chap. 392) Alcohol abuse is defined as repetitive problems in any one of four life areas that can be attributed to alcohol. The four life areas that can be affected by alcohol include social, interpersonal, legal, or occupational. In addition, an individual who repetitively engages in hazardous behaviors while under the influence of alcohol would be considered to suffer from alcohol abuse. However, this is to be differentiated from alcohol dependence. Alcohol dependence is defined in the DSM-IV as repeated alcohol-related difficulties in three of seven life areas and includes the development of tolerance and dependence. If tolerance or dependence is present, this predicts a more severe clinical course, and the presence of alcohol dependence decreases overall life span by about a decade. Only about 50% of individuals with alcohol abuse will continue to experience similar alcohol-related problems 3-5 years later, and only 10% will go onto develop alcohol dependence. The lifetime risk of alcohol dependence in most Western countries is about 10-15% in men and 5-8% in women. However, there may be higher rates in Ireland, France, and Scandinavian countries. In addition, native cultures appear to be especially susceptible to problems with alcohol dependence. This has been seen in Native Americans, Maoris, and the aboriginal tribes of Australia.
About 60% of the risk for alcohol use disorders is attributed to genetic influences. Children of alcoholics do have a higher risk of alcohol abuse and dependence; however, this risk is about 4 times higher, not 10. Identical twins also exhibit a higher risk of concurrent alcohol abuse and dependence when compared to fraternal twins. The genetic factors that appear to be most strongly linked to alcohol use disorders include genes that are linked to impulsivity, schizophrenia, and bipolar disorder. In addition, genes that affect alcohol metabolism or sensitivity to alcohol also contribute to the genetics of alcoholism. A mutation in aldehyde dehydrogenase that is more common in individuals of Asian descent results in intense flushing when alcohol is consumed and confers a decreased risk of alcohol dependence. Conversely, genetic variants that lead to a low sensitivity to alcohol increase the risk of subsequent alcohol abuse and dependence, as higher and higher doses of alcohol are required to achieve the same effects.
XI-78. The answer is B.(Chap. 392) Individuals with alcohol dependence are susceptible to alcohol withdrawal when alcohol intake is stopped abruptly. The individual in this case scenario is likely alcohol dependent given his large amount of alcohol intake on a daily basis. Symptoms of alcohol withdrawal can range from mild tremulousness to hallucinations, seizures, or the development of delirium tremens. Other clinical features of alcohol withdrawal include anxiety, insomnia, and autonomic nervous system overactivity manifested as tachycardia, tachypnea, elevated blood pressure, and fever. This patient exhibits symptoms of the more severe delirium tremens, with mental confusion, agitation, and fluctuating levels of consciousness. While minor symptoms of alcohol withdrawal may
begin as soon as 5-10 hours after cessation of alcohol intake, the symptoms do not peak for 48-72 hours, putting this patient in the appropriate time frame for alcohol withdrawal.
The best approach for the alcohol-dependent patient who abruptly stops all alcohol intake is to take a prophylactic approach and screen early for symptoms of alcohol withdrawal. Tools such as the Revised Clinical Institute for Withdrawal Assessment for Alcohol (CIWA-Ar) may help clinicians and nurses screen for the early development of symptoms and allow intervention before symptoms escalate. In this setting, most experts recommend the use of oral long-acting benzodiazepines such as chlordiazepoxide or diazepam beginning on the first day. However, in this case, the patient received no such treatment and is now experiencing severe alcohol withdrawal and delirium tremens. Intravenous medications that have a rapid onset of action and can be titrated for more aggressive symptom management are often employed in this setting. Thus, the use of IV lorazepam or diazepam is preferred in this patient. Following an initial bolus, repeated doses can be used in short intervals until the patient is calm but arousable. In some instances a continuous infusion may be required, although bolus dosing is preferred. In the most severe cases, propofol or barbiturates may be required, although the patient would most likely need to be intubated for airway protection with use of these medications.
The other options listed are not appropriate for initial management of this patient. Intravenous fluids and thiamine had been administered since hospital admission. Administration of glucose-containing fluids without thiamine in the alcohol-dependent patient can precipitate Wernicke's encephalopathy, which would present with ophthalmoparesis, ataxia, and encephalopathy. Given the patient's fever, an infectious etiology can be considered, and it would be appropriate to perform blood cultures in this patient. However, given the clear symptoms of alcohol withdrawal and lack of necrotizing pancreatitis on CT abdomen, empiric treatment with antibiotics is not required. Likewise, without focal neurologic findings, a head CT would be a low-yield diagnostic procedure that would be difficult to perform in the patient's current agitated condition and would only delay appropriate therapy. Finally, restraints are best avoided if the patient's safety can be ensured through the appropriate use of benzodiazepines, as restraints are only likely to make the patient's agitation worse and may lead to iatrogenic harm Haloperidol may have some sedative effect on the patient, but could lead to torsades de pointe arrhythmia as this patient is at risk for electrolyte deficiencies from his alcoholism and pancreatitis.
XI-79. The answer is D.(Chap. 392) In individuals recovering from alcoholism several medications may have a modest benefit in increasing abstinence rates. The two medications with the best risk-benefit ratio are acamprosate and naltrexone. Acamprosate inhibits NMDA receptors, decreasing symptoms of prolonged alcohol withdrawal. Naltrexone is an opioid antagonist than can be administered orally or as a monthly injection. It is thought to act by decreasing activity in the dopamine-rich ventral tegmental area of the brainstem and subsequently decreasing the pleasurable feelings associated with alcohol consumption. There is some research to suggest that the use of these medications in combination may be more effective than either one alone. Disulfiram is an aldehyde dehydrogenase inhibitor that has been used for many years in the treatment of alcoholism However, it is no longer a commonly used drug due to its many side effects and risks associated with treatment. The primary mechanism by which it acts is to create negative effects of vomiting and autonomic nervous system hyperactivity when alcohol is consumed concurrently with use of the medication. As it inhibits an enzyme that is part of the normal metabolism of alcohol, it allows the buildup of acetaldehyde, which creates these symptoms. Because of the autonomic side effects, it is contraindicated in individuals with hypertension, a history of stroke, heart disease, or diabetes mellitus.
XI-80. The answer is E.(Chap. 393) Prescription drug abuse has increased dramatically among all age groups and is strikingly common in teenagers. Since 2007, prescription opiates have passed marijuana as the most common illicit drugs that adolescents initially abuse. This has occurred at the same time as rates of prescription narcotic abuse have increased across all age groups. The annual prevalence of heroin abuse is approximately 0.14% of the population. In contrast, this prevalence is only one-third the rate of prescription opiate abuse. Among prescription narcotics, oxycodone is the single most commonly abused drug. Other common prescription narcotics that are abused include morphine and hydrocodone. Among health care professionals, meperidine and fentanyl are more frequently abused.
XI-81. The answer is B.(Chap. 393) Tolerance and withdrawal begin within 6-8 weeks of chronic daily opioid use. Tolerance develops not because of increased metabolism, but through a change in the pharmacodynamics of the drugs, requiring increasing doses to achieve the euphoric effects and prevent withdrawal. With the abrupt cessation of narcotics, acute withdrawal symptoms begin within 8-10 hours after the last dose. While the symptoms of narcotic withdrawal are noxious, they are not life threatening, as is the case with benzodiazepine or barbiturate withdrawal. The primary symptoms of opiate withdrawal are related to over activity of the autonomic nervous system. This manifests as increased lacrimation, rhinorrhea, and sweating. In addition, patients frequently will have diffuse piloerection (chill bumps), giving rise to the term "cold turkey." As withdrawal symptoms progress, patients appear restless with myalgias, nausea, vomiting, and diarrhea. Hypertension, hyperthermia, and tachypnea can occur as well. Hypotension is not a symptom of opioid withdrawal. A patient with known infection and new-onset hypotension should be evaluated for systemic infection, not withdrawal.
XI-82. The answer is E.(Chap. 393) The patient is presenting with an acute overdose of an unknown quantity of extended-release opioid medications taken with alcohol. When evaluating and treating a patient with an intention overdose, the first priority is to stabilize the patient's condition. The patient was appropriately given the opiate antagonist naloxone by emergency responders as the patient was near-apneic. In addition, the patient was also appropriately intubated and stabilized for transport to the hospital. In the emergency room, however, the patient remained hypotensive and unresponsive. At this point, the next step in stabilizing the patient is to support the blood pressure with bolus fluid resuscitation, and if the patient fails to respond, IV vasopressors would be required. Given his ongoing unresponsive state and the expected long duration of effect with a sustained-release preparation, it is appropriate to initiate a continuous infusion of naloxone. After a bolus dose, the expected onset of action is 1-2 minutes, but the duration of effect is only a few hours. Some care must be taken when giving naloxone as one only wants to reverse the respiratory and cardiovascular depression associated with the overdose. Particularly in chronic drug abusers, high doses of naloxone can precipitate the distressing symptoms of narcotic withdrawal. When long-acting preparations of opioids are taken, activated charcoal and gastric lavage are appropriate considerations to decrease the absorption of any undigested pills. While the patient is being stabilized from a cardiovascular and respiratory standpoint, it is important that the clinician consider if any other concurrent ingestion may have occurred that would affect the patient's outcome. As the patient is unable to provide any history and the overdose was not witnessed, one must not focus solely on the opioids. The appropriate approach is to perform a comprehensive toxicology evaluation that should include a urine drug screen, blood alcohol level, and acetaminophen levels, at a minimum. One could also consider sending for levels of aspirin or tricyclic antidepressants.
XI-83. The answer is C.(Chap. 394) Marijuana is the most commonly used illegal drug in the United States with over 6% of all individuals reporting current usage in 2009 (http://www.whitehousedrugpolicy.gov/publications/pdf7nsduh.pdf, accessed July 25, 2011). In part, the prevalence of marijuana use is related to the widespread belief that marijuana is thought to have few negative health effects. Acutely, marijuana causes a sense of relaxation and mild euphoria, not unlike that of alcohol intoxication. In addition, impaired judgment, cognition, and psychomotor performance are seen. Occasionally, acute intoxication can lead to negative emotional responses as well. A consensus about the chronic effects of marijuana usage is not clearly defined. Traditionally, marijuana usage has been linked with an "amotivational syndrome." While it is true that chronic users of marijuana may lose interest in day-to-day activities and spend more time using the drug, this is certainly not specific for marijuana uses, and a specific "amotivational syndrome" is not defined with chronic marijuana use. Other symptoms that have been attributed to chronic marijuana use that lack good evidence for causation include depression and maturational dysfunction. In individuals with a history of schizophrenia, however, chronic marijuana use has been associated with an increased risk of psychotic symptoms.
The physical effects of chronic marijuana use are also not clearly known. Acutely, marijuana causes increased heart rate, but tolerance for this effect occurs rapidly. Acute ingestion can also precipitate angina. The chronic effects on lung function are not known, as tobacco products are frequent confounders. Acute decreases in vital capacity and diffusion capacity are seen, but whether this translates into an increased risk of emphysema has not yet been determined. Most studies have not found an association with emphysema. A variety of other adverse physical effects have been described but not confirmed in a systematic fashion. This includes reports of low testosterone levels, decreased sperm count, impaired fetal growth, and chromosomal abnormalities.
Contrary to popular belief, chronic use of marijuana is associated with the development of tolerance as well as a withdrawal syndrome. Signs of physical tolerance include tolerance to the development of tachycardia and conjunctival injection. The psychological tolerance that develops is more prominent and predictable. This occurs rapidly, with individuals often seeking more potent compounds or smoking the drug more frequently. With cessation of marijuana use, a withdrawal syndrome can be demonstrated with irritability, anorexia, and sleep disturbance.
XI-84. The answer is E.(Chap. 395) Approximately 400,000 individuals die yearly in the United States as a result of cigarette smoking, accounting for about 20% of all deaths. While heart disease, lung cancer, and chronic obstructive pulmonary disease are most commonly connected with tobacco-related deaths, multiple cancers have also been associated with cigarette smoking. Of all cancers, cancers of the lung, oropharynx, and larynx have the strongest associations. The relative risk of lung cancer in current male cigarette smokers is as high as 23.3. However, the relative risk of lung cancer is only 12.7 among current female smokers. Other cancers that have been associated with cigarette smoking include esophageal, bladder, kidney, pancreatic, stomach, cervical, and acute myeloid leukemia. Postmenopausal breast cancer is not associated with current cigarette use, although there may be a link with premenopausal breast cancer that has not yet been fully determined.
XI-85. The answer is B.(Chap. 395) Smoking cessation is vitally important in promoting health and preventing adverse outcomes related to cigarette use. However, nicotine is a remarkably addictive substance, and most smokers require several attempts at smoking cessation prior to success. It is estimated that 33% of current smokers attempt to quit each year, with 90% of unassisted attempts at
smoking cessation resulting in failure. Even with the appropriate support and best medical treatments available, sustained quit rates of 20-30% are typical. Short counseling sessions by a physician alone do increase quit rates. Therefore, questions about current tobacco use and prior quit attempts should be part of every office visit. Even when patients do not express the desire to stop smoking, they should be encouraged to consider the potential benefits of smoking cessation. As part of counseling, the physician should negotiate a quit date with the patient, typically 2 or 3 weeks after the appointment, and follow-up phone calls may be helpful. However, most often counseling should be combined with pharmacologic interventions to improve quit rates. A variety of options are available, and the most commonly used treatments are nicotine replacement therapy, bupropion, and varenicline. In this patient with a history of depression that is inadequately treated, combined therapy with bupropion and nicotine replacement would have the greatest likelihood of success. Bupropion is an antidepressant medication that has been studied for smoking cessation in randomized clinical trials. Pretreatment with bupropion for 1-2 weeks prior to the quit date increases success. Concomitant use of nicotine replacement therapy can be administered in a variety of forms including patches, gum, lozenges, and nasal or oral inhalers. Some programs advocate combining patches with a more rapidly acting nicotine product that can alleviate acute cravings for nicotine. Varenicline is a recently introduced medication that acts as a partial agonist at the nicotinic acetylcholine receptor. Concomitant nicotine administration is not felt to be helpful. Use of varenicline in this patient is contraindicated given the patient's history of untreated depression. Varenicline has been associated with severe psychiatric symptoms, and there are reports of suicide that have been related to its use.
XI-86. The answer is D.(Chap. 395) Cigarette smoking is associated with early mortality from a variety of causes including cardiovascular, respiratory, cerebrovascular, and oncologic. It is also associated with increased complications during pregnancy (premature rupture of membranes, placenta previa, abruption placenta), delay in healing of peptic ulcers, osteoporosis, cataracts, macular degeneration, cholecystitis in women, and impotence in men. Children born to smoking mothers are more likely to have preterm delivery, higher perinatal mortality, higher rates of infant respiratory distress, and higher rates of sudden infant death. Moreover, 400,000 individuals die prematurely each year in the United States from cigarette use, representing 1 out of every 5 deaths.
XI-87. The answer is B.(Chap. 395) Smokers regulate their blood levels of nicotine by adjusting the frequency and intensity of their tobacco use. Smokers can compensate for the lower levels of nicotine in low-yield cigarettes by smoking more cigarettes or by adjusting their smoking technique with a deeper inhalation and breath hold. Therefore, smoking low-yield cigarettes is not a reasonable alternative to smoking cessation. Moreover, there is no difference in the harmful physical effects of smoking or in the potential for drug interactions. Finally, although not definitively proven, there is some thought that the rise in adenocarcinoma of the lung over the past 50 years is associated with introduction of the low-tar cigarette and the resultant change in smoking behavior associated with this.
SECTION XII Dermatology
QUESTION
DIRECTIONS: Choose the one best response to each question.
XII-1. A 34-year-old woman seeks evaluation for a skin lesion. On examination, the lesion is present on the extensor surface of the right elbow. It measures 2.4 cm in diameter and is raised, with a flat top and distinct edge. Overlying the lesion is an excess accumulation of stratum cornea. Further examination reveals several smaller lesions also located on extensor surfaces. Which term best characterizes the primary lesion for which the patient is seeking evaluation?
A. Macule with lichenification
B. Patch with a scale
C. Plaque with a crust
D. Plaque with a scale
E. Tumor
XII-2. What term is used in dermatology to describe a coin-shaped lesion?
A. Herpetiform
B. Lichenoid
C. Morbilliform
D. Nummular
E. Polycyclic
XII-3. A 5-year-old boy is brought in by his mother complaining of approximately 6 months of itching and scaling of the skin inside the elbows (see Figure XII-3). The area gets red occasionally and improves with over-the-counter topical steroid creams. There is no fever, chills, night sweats, or red streaks ascending the arm. The family has a pet cat and lives in a clean apartment. All of the following statements concerning this child are true EXCEPT:

FIGURE XII-3 (see Color Atlas) (Courtesy of Robert Swerlick, MD; with permission.)
A. Both of his parents likely have a history of atopic dermatitis.
B. He likely has a history of asthma or atopic rhinitis.
C. His serum IgE levels are elevated.
D. He has a greater than 70% chance of spontaneous resolution.
E. His lesions will likely respond to topical tacrolimus.
XII-4. A 63-year-old woman has a 5-year history of psoriasis involving her elbows that has been controlled with topical glucocorticoids and a vitamin D analogue. However, in the past 9–12 months she has developed worsening and new lesions involving her knees, gluteal regions, and scalp. She is increasingly uncomfortable and has noted swelling of her digits with pain and stiffness. She is up to date on all cancer screening and has no sign of systemic infection. Her physical examination is only notable for the psoriatic plaques that are red and scaling, and swollen, tender DIPs on both hands. All of the following therapies are indicated for worsening widespread systemic psoriatic disease EXCEPT:
A. Alefacept
B. Cyclosporine
C. Infliximab
D. Methotrexate
E. Prednisone
XII-5. A 67-year-old man presents with complaints of diffuse rash with blistering. The lesions began as pruritic plaques distributed on the trunk and abdomen. Lesions are now appearing on the flexor surfaces of the arms. Some of the lesions have developed into tense blisters that rupture. As the lesions have healed, no scarring is present. A photo of the patient’s rash is shown in Figure XII-5. What would be the expected finding on biopsy of the lesion?
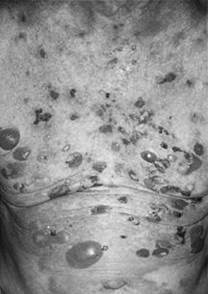
FIGURE XII-5 (see Color Atlas) (Courtesy of the Yale Resident’s Slide Collection; with permission.)
A. Cell surface deposition of IgG on keratinocytes
B. Cell surface deposition of IgG and C3 on keratinocytes
C. Granular deposits of IgA in dermal papillae
D. Linear band deposition of IgA in the epidermal basement membrane zone
E. Linear band deposition of IgG and/or C3 in the epidermal basement membrane zone
XII-6. A 24-year-old woman seeks evaluation for a rash that is present diffusely on her back, buttocks, elbows, and knees. The rash began abruptly and the patient is complaining of severe pruritus and burning associated with the rash. A biopsy of the rash demonstrates neutrophilic dermatitis within the dermal papillae, and immunofluorescence highlights granular deposition of IgA in the papillary dermis and along the epidermal basement membrane zone. What treatment do you recommend for this patient?
A. Dapsone 100 mg daily
B. Gluten-free diet
C. Prednisone 40 mg daily
D. A and B
E. All of the above
XII-7. A patient presents to you for evaluation of ear lesions worsening over the last 6–9 months. Each lesion began as a red papule with a thick adherent scale (see Figure XII-7). Since that time, they have progressed to the current pictured lesions with variable coloration, raised borders, and scars. There has been no improvement with use of topical glucocorticoids, which the patient borrowed from a friend. What is the best course of action for this patient at this time?

FIGURE XII-7 (see Color Atlas)
A. Aminoquinoline antimalarials
B. Azathioprine
C. Systemic glucocorticoids
D. Vitamin E ointment
E. Wide surgical excision with regional lymph node dissection
XII-8. A 55-year-old man presents with fever and a blistering skin rash that has developed after taking allopurinol for gout. The patient also is complaining of a sore throat and painful watery eyes. On examination, the patient is found to have blisters developing over a targetoid lesion with oral mucosal involvement. The estimated body surface area that is currently affected is 33%. Which of the following statements regarding this patient’s diagnosis and treatment are TRUE?
A. Immediate treatment with intravenous immunoglobulin will decrease the extent of the disease
and improve mortality.
B. Long-term treatment with glucocorticoids is required to prevent relapse of the disease.
C. The expected mortality rate from this syndrome is about 30%.
D. The most common drug to cause this syndrome is penicillin.
E. Younger individuals have a higher mortality than older individuals with this syndrome.
XII-9. A 32-year-old man receives amoxicillin/clavulanate for presumed bacterial sinusitis. One week later he presents with a diffuse itchy rash (see Figure XII-9). His mucous membranes are normal. Which of the following is the most likely diagnosis?

FIGURE XII-9 (see Color Atlas)
A. Morbilliform drug eruption
B. Pemphigus vulgaris
C. Stevens-Johnson syndrome
D. Toxic shock syndrome
E. Urticaria
XII-10. A 22-year-old woman comes to your office concerned about sun exposure. She brings a few sunblock creams into your office and wants to know which one is best for preventing wrinkling and blotchiness. She is less concerned about sunburn because she is trying to get a better tan. Blocking which ultraviolet rays will achieve her desired result?
A. UV-A
B. UV-B
C. Both UV-A and UV-B equally
D. Neither UV-A nor UV-B
XII-11. A 45-year-old patient with HIV/AIDS presents to the emergency department. He complains of a rash that has been slowly spreading up his right arm and is now evident on his chest and back. The rash consists of small nodules that have a reddish-blue appearance. Some of them are ulcerated, but there is minimal fluctuance or drainage. He is unsure when these began. He notes no foreign travel or unusual exposures. He is homeless and unemployed, but occasionally gets work as a day laborer doing landscaping and digging. A culture of a skin lesion grows a Mycobacterium in 5 days. Which of the following is the most likely organism?
A. M. abscessus
B. M. avium
C. M. kansasii
D. M. marinum
E. M. ulcerans
XII-12. A 22-year-old man presents to the emergency department complaining of generalized malaise and rash. The patient has a history of illicit drug use with intranasal heroin and cocaine. He admits to engaging in unprotected sexual intercourse with men in exchange for drugs. He was negative for the HIV
virus 8 weeks previously. He has a prior history of syphilis and gonorrhea that were treated appropriately 2 years previously. Following treatment, his rapid plasma reagin test fell to a titer of 1:8 from a high of 1:128 after 12 months. On physical examination, the patient has normal vital signs without fever. He is well developed and has no wasting. Diffuse lymphadenopathy measuring up to 2.5 cm is palpable in the cervical, axillary, and femoral areas. Genital examination shows no ulcerations or lesions. The rash is shown in Figure XII-12. Which test is most likely to yield the appropriate diagnosis in this patient?
A. Fluorescent treponemal antibody test
B. HIV antibody
C. HIV viral load
D. Rapid plasma reagin test
E. Venereal Disease Research Laboratory test

FIGURE XII-12 (see Color Atlas) (Courtesy of Jill McKenzie and Christina Marra.)
XII-13. While on a medical mission to the Ivory Coast, you are asked to see a 17-year-old boy with a large skin lesion on his forearm (see Figure XII-13). The lesion began as a small bump about 3 weeks ago and has grown to the size of a raspberry. He has tender axillary adenopathy on the ipsilateral side but no other physical findings. His siblings report similar lesions that healed after about 6 months. Which of the following is the most appropriate therapy?

FIGURE XII-13 (see Color Atlas)
A. Albendazole
B. Ivermectin
C. Penicillin
D. Praziquantel
E. Vancomycin
XII-14. Infection by what organism causes the rash shown in Figure XII-14?

FIGURE XII-14 (see Color Atlas) (Courtesy of Vijay K. Sikand, MD; with permission.)
A. Anaplasma phagocytophilum
B. Bartonella henselae
C. Borrelia burgdorferi
D. Ehrlichia chaffeensis
E. Rickettsia rickettsii
XII-15. A 36-year-old man with HIV/AIDS (CD4+ lymphocyte count = 112/μL) develops a scaly, waxy, yellowish, patchy, crusty, pruritic rash on and around his nose. The rest of his skin examination is normal. Which of the following is the most likely diagnosis?
A. Molluscum contagiosum
B. Kaposi’s sarcoma
C. Psoriasis
D. Reactivation herpes zoster
E. Seborrheic dermatitis
XII-16. A 34-year-old man seeks the advice of his primary care physician because of an asymptomatic rash on his chest. There are coalescing light-brown to salmon-colored macules present on the chest. A scraping of the lesions is viewed after a wet preparation with 10% potassium hydroxide solution. There are both hyphal and spore forms present, giving the slide an appearance of “spaghetti and meatballs.” In addition, the lesions fluoresce to a yellow-green appearance under a Wood’s lamp. Tinea versicolor is diagnosed. Which of the following microorganisms is responsible for this skin infection?
A. Fusarium solani
B. Malassezia furfur
C. Penicillium marneffei
D. Sporothrix schenckii
E. Trichophyton rubrum
XII-17. A 19-year-old college freshman comes to the clinic complaining of blistering skin lesions on the back of his hands and arms that are painful. He’s noticed these occasionally during his childhood, and they were often precipitated by sunlight and healed with scarring. He now notices that since starting college they are more frequent, and often occur after drunken parties. His hands and forearms have numerous hypopigmented scars that he says are from previous episodes. The skin over the back of his hands appears thick and coarse. Otherwise his review of systems and physical examination is normal. The lesions on his hands are shown in Figure XII-17. Which of the following tests will most likely yield the correct diagnosis?

FIGURE XII-17 (see Color Atlas) (Courtesy of Dr. Karl E. Anderson; with permission.)
A. ANA
B. Anti-SCL-70
C. Plasma cortisol
D. Plasma porphyrin
E. Urine porphobilinogen
XII-18. A 22-year-old male comes to the clinic reporting severe penile itching and new skin lesions. His last sexual encounter was unprotected sex 3 weeks prior with a new female partner in her bed. He has not seen her since. Over the last 3 days he’s noticed new lesions on his penis and scrotum. The lesions are extremely pruritic, particularly at night and after a shower. His physical examination is shown in Figure XII-18. Which of the following is the best therapy?
A. Ceftriaxone plus azithromycin
B. Metronidazole
C. Penicillin G
D. Permethrin
E. Vancomycin

FIGURE XII-18 (see Color Atlas)
ANS
XII-1. The answer is D. (Chap. 51) Rashes and skin lesions are the most common reasons for visits to primary care physicians. Accurately characterizing a skin lesion is important for determining the underlying cause of the disease. Four basic features that are important when describing a skin lesion are the distribution, types of primary and secondary lesions, shape, and arrangement of lesions. The primary description of a skin lesion takes into account size, whether the lesion is raised or flat, and whether the lesion is fluid filled. Raised lesions can be papules, nodules, tumors, or plaques. A plaque is a raised lesion with a flat top that measures more than 1 cm in diameter. The edges may be distinct or gradually blend in with the surrounding skin. Papules, nodules, and tumors are similar raised solid lesions of the skin. These lesions differ only by size, with papules being smaller than 0.5 cm, nodules measuring 0.5–5.0 cm, and tumors measuring more than 5 cm. Macules and patches are not raised and also differ only by size, with macules being less than 2 cm and patches being greater than 2 cm. Vesicles are small (<0.5 cm) fluid-filled lesions, and pustules are vesicles containing leukocytes. Larger fluid-filled lesions are called bullae. A secondary description of a skin lesion takes into account features of the lesion. An excess accumulation of stratum corneum on a skin lesion is called a scale. Thus, this patient would be characterized as having a plaque with a scale. Other secondary descriptors include lichenification, which refers to a distinctive thickening of the skin that accentuates skinfold markings, and crusting, which refers to dried body fluids. In addition, the lesion may have erosions, ulceration, excoriation, atrophy, or scarring.
XII-2. The answer is D. (Chap. 51) Characteristic terms are used in dermatology to describe a skin
lesion. Nummular lesions are coin shaped and are closely related to annular lesions, which are ring shaped. A polycyclic eruption consists of a configuration of skin lesions that coalesce to form a ring or incomplete rings. Herpetiform lesions are grouped in a fashion that is seen in herpes simplex virus infection, whereas morbilliform lesions are generalized macules or papules that are similar to those seen in a measles eruption. Lichenoid rashes are violaceous lesions that resemble those seen in lichen planus.
XII-3. The answer is D. (Chap. 52) These lesions are typical examples of childhood atopic dermatitis, the cutaneous expression of the atopic state. Over 75% of patients present by 5 years of age, and a similar proportion has concomitant asthma and/or allergic rhinitis. There is a strong genetic predisposition. Over 80% of children whose parents both have atopic dermatitis will have similar skin findings; the prevalence is approximately 50% when one parent is affected. In addition to the antecubital fossae, the face, neck, and other extensor surfaces are commonly affected. The typical course involves exacerbations and remissions. In the adult form, the disease is often localized lichen simplex chronicus or hand eczema. Treatment of atopic dermatitis involves adequate moisturizing, topical anti-inflammatories, and avoidance of secondary bacterial infection. Topical tacrolimus and pimecrolimus are approved as therapy. They do not cause some of the complications of topical corticosteroids, but recent reports have raised the concern of a potentially increased risk of lymphoma. Children with atopic dermatitis may have spontaneous resolution, but about 40% of children with symptoms will have dermatitis as adults. Interestingly, for unknown reasons the worldwide prevalence of atopic dermatitis is increasing.
XII-4. The answer is E. (Chap. 52) All patients with psoriasis should be advised to avoid excessive drying of the skin and maintain hydration. Secondary bacterial infection should be suspected with local worsening and treated appropriately. Topical glucocorticoids often cause skin atrophy and lose effectiveness over time. Topical vitamin D analogues and retinoids have effectively replaced topical coal tar, salicylic acid, and anthralin as local adjunctive therapies. UV-A (with psoralen) and/or UV-B light is an effective therapy for widespread psoriasis in many cases. These therapies may be associated with an increased risk of skin cancer, particularly in patients who are immunocompromised. Methotrexate is often effective in patients with psoriatic arthritis (up to 30% of patients with psoriasis). Cyclosporine and other modulators of T-cell mediated immunity are effective in psoriasis. Alefacept is an intramuscular biologic that is anti-CD2 and is indicated in psoriasis. It may cause lymphopenia, increased risk of infection, or secondary malignancy. Infliximab, etanercept, and adalimumab are anti-TNF biologics indicated for use in psoriasis arthritis (etanercept is indicated for psoriasis). They are associated with an increased risk of serious systemic infection, neurologic events (progressive multifocal leukoencephalopathy), and hypersensitivity reactions. Oral glucocorticoids should not be used for the treatment of psoriasis due to the potential for developing life-threatening pustular psoriasis when the therapy is discontinued.
XII-5. The answer is E. (Chap. 54) Bullous pemphigoid is an autoimmune skin disease associated with the development of tense vesicles and bullae on erythematous bases. The disease is more common in elderly individuals and typically begins as urticarial plaques that are located on the lower abdomen, groin, and flexor surfaces of the extremities. These lesions often evolve to tense bullae on erythematous or normal-appearing skin. Oral mucosal lesions can occur, and pruritus is variable from none to severe. The blisters often rupture with secondary erosions and crusting. Without secondary trauma, these
lesions will heal without scarring. Biopsy of early lesions shows subepidermal blisters with a variable inflammatory infiltrate. Lesions on an erythematous base demonstrate eosinophilic infiltrates, whereas lesions on normal skin have minimal perivascular infiltrate only. Direct immunofluorescence shows linear deposits of IgG and C3 along the epidermal basement membranes. In about 70% of individuals, autoantibodies can be found that bind to the epidermal basement membrane. The disease tends to be chronic with relapses and remissions over a period of months to years. The treatment of choice is systemic glucocorticoids at doses of prednisone equivalent to 0.75–1 mg/kg daily.
XII-6. The answer is D. (Chap. 54) Dermatitis herpetiformis (DH) is an immunologic skin disorder characterized by severe pruritus with skin lesions symmetrically distributed along the extensor surfaces, buttocks, back, scalp, and posterior neck. The lesions of DH may be papular, papulovesicular, or urticarial plaques. Because of the severity of the associated pruritus, many patients do not exhibit the primary skin lesions but have excoriations and crusted papules. Burning and stinging are also frequently reported along with the pruritus, and these symptoms are present prior to the manifestation of skin lesions. Almost all patients have an associated gluten-sensitive enteropathy, although it may be clinically unrecognized on presentation. Pathologically, the lesions demonstrate a neutrophilic inflammatory infiltrate in the dermal papillae. On immunofluorescence, granular deposits of IgA are found in the papillary dermis and along the epidermal basement membrane. The primary treatment of DH is dapsone at doses of 50–200 mg daily with most patients reporting remarkable improvement within 24–48 hours. At doses greater than 100 mg daily, one must pay close attention to side effects as methemoglobinemia and hemolysis frequently occur. In addition to dapsone, gluten-free diets are recommended. However, many months of the diet are required to achieve a clinical benefit and are not recommended as the sole treatment. Corticosteroids are not used in the treatment of DH.
XII-7. The answer is A. (Chap. 54) The patient has discoid lupus erythematosus (DLE) or chronic cutaneous lupus erythematosus. It is characterized by discrete lesions most often on the face, scalp, or ears. The lesions are usually erythematous papules or plaques with a thick scale that occludes hair follicles. The lesions persist for years and grow slowly. Less than 10% of patients with DLE meet the criteria for systemic lupus erythematosus (SLE), although skin lesions are common in patients with SLE. Chronically, the lesions evolve to look similar to the one pictured. Treatment consists of topical or intralesional glucocorticoids. If that is ineffective, systemic therapy with an aminoquinoline antimalarial may be indicated. Systemic glucocorticoids or immunosuppressives are not indicated for localized disease. Although malignant melanoma may take on myriad appearances, the location, progress, and description of this lesion is more suggestive of discoid lupus; therefore, surgical excision and lymph node dissection are not indicated at this time. Vitamin E ointment has no proven role in the treatment of DLE.
XII-8. The answer is C. (Chap. 55) Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are the most dreaded drug reactions and are characterized by diffuse blistering and epidermal necrosis with skin detachment. In both syndromes, the lesions typically begin with blisters developing over target lesions with mucosal involvement. In SJS, the amount of skin detachment is between 10% and 30% with the more severe TEN associated with skin detachment of more than 30%. Mortality is directly related to the amount of skin detachment with a mortality of about 10% in SJS and 30% in TEN. Other risk factors for mortality in SJS/TEN include older age and intestinal or pulmonary involvement. The most common drugs to cause SJS/TEN are sulfonamides, allopurinol, nevirapine,
lamotrigine, aromatic anticonvulsants, and the oxicam nonsteroidal anti-inflammatory drugs (NSAIDs). There is no evidence that any therapy changes outcomes in SJS or TEN. Clearly, immediate cessation of the offending agent is necessary. Supportive therapy to prevent secondary infections is important. In many instances, these patients are treated in burn wards. Systemic corticosteroids may be useful for the short-term treatment of SJS/TEN, but these drugs increase long-term complications and have a higher associated mortality. Early data suggested that intravenous immunoglobulin (IVIG) may be helpful, but more recent studies have not shown benefit. Future studies are required to determine the role of IVIG in the treatment of SJS/TEN.
XII-9. The answer is A. (Chap. 55) Morbilliform drug eruptions are the most common drug reactions. They typically begin on the trunk and consist of symmetric macules and papules that may become confluent. Moderate to severe pruritus is common. In contrast to Stevens-Johnson syndrome and toxic shock syndrome, involvement of the mucous membranes is uncommon. The principal differential diagnosis is viral exanthem, particularly in children. The rash usually develops within 1 week of initiation of therapy and resolves with discontinuation within 2 weeks. The most common drugs that cause morbilliform eruptions include penicillin derivatives, allopurinol, sulfonamides, and nonsteroidal anti-inflammatories. Urticaria consists of superficial well-defined wheals that are pruritic. Penicillins may cause IgE-mediated urticaria. Pemphigus is an autoimmune bullous disease of the skin and mucous membranes that is rarely associated with drugs such as penicillin.
XII-10. The answer is A. (Chap. 56) The UV spectrum reaching the earth is arbitrarily divided into two major segments: UV-A and UV-B. The outermost epidermal layer, the stratum corneum, is a major absorber of UV-B, and less than 10% of incident UV-B wavelengths penetrate through the epidermis to the dermis. In contrast, UV-A readily penetrates to the dermis. Photons in the UV-B are 1000-fold more efficient than photons in the UV-A in evoking the sunburn response. UV-B is primarily responsible for the sunburn response and for vitamin D photochemistry. UV-A is important in the pathogenesis of photoaging in human skin.
XII-11. The answer is A. (Chap. 167) Nontuberculous mycobacteria (NTM) were originally classified into “fast-growers” and “slow-growers” based on the length of time they took to grow in culture. Although more sophisticated tests have been developed, this classification scheme is still used and is of some benefit to the clinician. Fast-growing NTM include M. abscessus, M. fortuitum, and M. chelonae. They will typically take 7 days or less to grow on standard media, allowing relatively fast identification and drug-resistance testing. Slow-growing NTM include M. avium, M. marinum, M. ulcerans, and M. kansasii. They often require special growth media and therefore a high pretest suspicion. The patient described likely has a cutaneous infection from one of the “fast-growing” NTM, which could be diagnosed with tissue biopsy, Gram stain, and culture.
XII-12. The answer is D. (Chap. 169) This vignette presents a patient with symptoms consistent with secondary syphilis. The causative organism of syphilis is Treponema pallidum, and it can penetrate normal skin to disseminate via the bloodstream long before the appearance of the typical skin lesion of primary syphilis. This lesion appears at the initial site of inoculation only after a period of 4–6 weeks. It will heal spontaneously, and symptoms of secondary syphilis begin approximately 6–8 weeks after it heals. However, as much as 15% of individuals will have evidence of healing chancres at the time of the manifestation of secondary syphilis. The primary manifestations of secondary syphilis are a generalized rash with generalized lymphadenopathy. The skin rash of secondary syphilis is most
commonly macular or maculopapular and nonpuritic with a pink color. The rash begins on the trunk and upper extremities and classically progresses to involve the palms and soles. Ten percent of individuals with secondary syphilis also exhibit condylomata lata, which are papular lesions that develop in intertriginous areas. It is notable that the skin lesions of secondary syphilis do harbor bacteria and are infectious. A variety of constitutional symptoms can be present in secondary syphilis including malaise, fever, weight loss, sore throat, and headache.
Diagnosis of secondary syphilis in this patient with a prior diagnosis of syphilis is best accomplished by means of nontreponemal antibody testing. There are two common nontreponemal antibody tests: the rapid plasma reagin (RPR) test and the Venereal Disease Research Laboratory (VDRL) test. This patient’s prior syphilis infection was diagnosed and treated based on a positive RPR, which demonstrated the appropriate fourfold decrease in titers after appropriate therapy. As VDRL titers do not directly correspond to RPR titers, it is recommended that sequential testing be performed via the same nontreponemal test. In this case, that would be the RPR, as the VDRL would be difficult to interpret in the absence of previous titers. The fluorescent treponemal antibody test (FTA-Abs) is a specific treponemal antibody test. It does cross-react in the presence of other treponemal infections such as yaws or pinta. More importantly in this case, it remains positive after treatment of prior infection and lacks the ability to differentiate between new and past infections. Primary HIV infection is certainly a concern in this patient given his risk factors. It can present similarly with a fever, rash, malaise, and generalized lymphadenopathy. The rash of primary HIV infection is also a maculopapular disseminated rash, but it is much less likely to affect the palms and soles. Acute HIV infection would be best diagnosed by obtaining an HIV viral load and would be reasonable to consider as additional testing in this patient, but would not yield the appropriate diagnosis. Given his recent negative antibody testing, the HIV antibody test would not likely be positive in the setting of recent infection.
XII-13. The answer is C. (Chap. 170) The lesion shown is typical of primary yaws skin infection caused by the endemic treponeme T. pallidum subsp. Pertenue. Yaws remains a health problem in parts of West Africa (including Ivory Coast and Ghana), Central Africa Republic, rural Congo, Indonesia, Papua New Guinea, Haiti, and parts of South America. India has not had a reported new case since 2003. As in syphilis, endemic treponemal infections typically have primary, secondary, and late stages. Yaws (also known as pian, framboesia, or bouba) is characterized by a primary raspberry-like lesion at the site of inoculation. Early skin lesions are infectious by contact and may persist for months. Cutaneous relapses are common, and late disease affects approximately 10% of patients with destructive skin, bone, and joint lesions. Primary infection is often associated with regional lymphadenopathy. Late yaws is characterized by gummas of the bones and skin. Destruction of the nose, maxilla, palate, and pharynx similar to leprosy and leishmaniasis may occur. Darkfield examination is diagnostic, and because of cross-reactivity the same serologic tests used for syphilis are positive. Therapy of yaws is based on treatment of syphilis because there are no controlled treatment trials of yaws. Penicillin, doxycycline, and tetracycline are thought to be effective therapies. Albendazole, ivermectin, and praziquantel are used for a variety of worm infections.
XII-14. The answer is C. (Chap. 174) The picture shows the characteristic rash of erythema migrans, the defining lesion of Lyme disease caused by Borrelia burgdorferi. Erythema migrans appears at the site of the tick bite within 3–32 days following the initial bite. It typically begins as a red macule or papule and expands slowly to form an annular lesion. As the lesion gets larger, the classic targetoid
appearance develops with a bright red outer ring as well as ongoing erythema at the central lesion with clearing in between. The most common sites of erythema migrans are the classic locations of tick bites, including the groin, axilla, and thigh. The presence of this lesion in an endemic area for Lyme disease is an indication for treatment and does not require serologic confirmation.
Anaplasma phagocytophilum is the causative organism of human granulocytic anaplasmosis. This rickettsial disease is also transmitted through a tick bite and is prevalent in the uppe
Date: 2016-04-22; view: 1066
| <== previous page | | | next page ==> |
| TABLE XI-42 Initial Symptoms of MS | | | GRINGOTTS BREAK-IN LATEST |