
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
TABLE IV-114 Risk Factors for Active Tuberculosis Among Persons Who Have Been Infected With Tubercle Bacilli 30 page
A. Creatinine clearance
B. Glucose tolerance test
C. Serum creatinine level
D. Ultrasonography
E. Urine albumin
X-55. Alteration in which of the following substance levels is the first defense against hypoglycemia?
A. Cortisol
B. Epinephrine
C. Glucagon
D. Insulin
E. Insulin-like growth factor
X-56. A 25-year-old health care worker is seen for evaluation of recurrent hypoglycemia. She has had several episodes at work over the past year in which she feels shaky, anxious, and sweaty, and when she measures her finger stick glucose, it is 40–55 mg/dL. She drinks orange juice and feels better. These episodes have not happened outside the work environment. Aside from oral contraceptives, she takes no medications and is otherwise healthy. Which of the following tests is most likely to demonstrate the underlying cause of her hypoglycemia?
A. Measurement of insulin-like growth factor 1
B. Measurement of fasting insulin and glucose levels
C. Measurement of fasting insulin, glucose, and C-peptide levels
D. Measurement of insulin, glucose, and C-peptide levels during a symptomatic episode
E. Measurement of plasma cortisol
X-57. All of the following statements regarding hypoglycemia in diabetes mellitus are true EXCEPT:
A. Individuals with type 2 diabetes mellitus experience less hypoglycemia than those with type 1
diabetes mellitus.
B. From 2–4% of deaths in type 1 diabetes mellitus are directly attributable to hypoglycemia.
C. Recurrent episodes of hypoglycemia predispose to the development of autonomic failure with
defective glucose counterregulation and hypoglycemia unawareness.
D. The average person with type 1 diabetes mellitus has two episodes of symptomatic
hypoglycemia weekly.
E. Thiazolidinediones and metformin cause hypoglycemia more frequently than sulfonylureas.
X-58. A 58-year-old man is seen in his primary care physician’s office for evaluation of bilateral breast enlargement. This has been present for several months and is accompanied by mild pain in both breasts. He reports no other symptoms. His other medical conditions include coronary artery disease with a history of congestive heart failure, atrial fibrillation, obesity, and type 2 diabetes mellitus. His current medications include lisinopril, spironolactone, furosemide, insulin, and digoxin. He denies illicit drug use and has fathered three children. Examination confirms bilateral breast enlargement with palpable glandular tissue that measures 2 cm bilaterally. Which of the following statements regarding his gynecomastia is true?
A. He should be referred for mammography to rule out breast cancer.
B. His gynecomastia is most likely due to obesity with adipose tissue present in the breast.
C. Serum testosterone, LH, and FSH should be measured to evaluate for androgen insensitivity.
D. Spironolactone should be discontinued and exam followed for regression.
E. Liver function testing should be performed to screen for cirrhosis.
X-59. All the following drugs may interfere with testicular function EXCEPT:
A. Cyclophosphamide
B. Ketoconazole
C. Metoprolol
D. Prednisone
E. Spironolactone
X-60. Clinical signs and findings of the presence of ovulation include all of the following EXCEPT:
A. Detection of urinary LH surge
B. Estrogen peak during secretory phase of menstrual cycle
C. Increase in basal body temperature more than 0.5°F in the second half of the menstrual cycle
D. Presence of mittelschmerz
E. Progesterone level above 5 ng/mL 7 days before expected menses
X-61. A couple has been married for 5 years and has attempted to conceive a child for the last 12 months. Despite regular intercourse they have not achieved pregnancy. They are both 32 years of age and have no medical problems. Neither partner is taking medications. Which of the following is the most likely cause of their infertility?
A. Endometriosis
B. Male causes
C. Ovulatory dysfunction
D. Tubal defect
E. Unexplained
X-62. A couple seeks advice regarding infertility. The female partner is 35 years old. She has never been pregnant and took oral contraceptive pills from age 20 until age 34. It is now 16 months since she discontinued her oral contraceptives. She is having menstrual cycles approximately once every 35 days, but occasionally will go as long as 60 days between cycles. Most months, she develops breast tenderness about 2–3 weeks after the start of her menstrual cycle. When she was in college, she was treated for Neisseria gonorrhoeae that was diagnosed when she presented to the student health center with a fever and pelvic pain. She otherwise has no medical history. She works about 60 hours weekly as a corporate attorney and exercises daily. She drinks coffee daily and alcohol on social occasions only. Her body mass index (BMI) is 19.8 kg/m2. Her husband, who is 39 years old, accompanies her to the evaluation. He also has never had children. He was married previously from the ages of 24–28. He and his prior wife attempted to conceive for about 15 months, but were unsuccessful. At that time, he was smoking marijuana on a daily basis and attributed their lack of success to his drug use. He has now been completely free of drugs for 9 years. He suffers from hypertension and is treated with lisinopril 10 mg daily. He is not obese (BMI, 23.7 kg/m2). They request evaluation for their infertility and help with conception. Which of the following statements is true in regard to their infertility and likelihood of success in conception?
A. Determination of ovulation is not necessary in the female partner as most of her cycles occur regularly, and she develops breast tenderness midcycle, which is indicative of ovulation.
B. Lisinopril should be discontinued immediately because of the risk of birth defects associated
with its use.
C. The female partner should be assessed for tubal patency by a hysterosalpingogram. If significant
scarring is found, in vitro fertilization should be strongly considered to decrease the risk of ectopic
pregnancy.
D. The prolonged use of oral contraceptives for more than 10 years has increased the risk of
anovulation and infertility.
E. The use of marijuana by the male partner is directly toxic to sperm motility, and this is the likely
cause of their infertility.
X-63. Which of the following forms of contraception have theoretical efficacy of more than 90%?
A. Condoms
B. Intrauterine devices
C. Oral contraceptives
D. Spermicides
E. All of the above
X-64. A 30-year-old male, the father of three children, has had progressive breast enlargement during the last 6 months. He does not use any drugs. Laboratory evaluation reveals that both LH and testosterone are low. Further evaluation of this patient should include which of the following?
A. 24-hour urine collection for the measurement of 17 ketosteroids
B. Blood sampling for serum glutamic-oxaloacetic transaminase (SGOT) and serum alkaline
phosphatase and bilirubin levels
C. Breast biopsy
D. Karyotype analysis to exclude Klinefelter’s syndrome
E. Measurement of estradiol and human chorionic gonadotropin (hCG) levels
X-65. The Women’s Health Initiative study investigated hormonal therapy in postmenopausal women. The study was stopped early due to increased risk of which of the following diseases in the estrogen-only arm?
A. Deep venous thrombosis
B. Endometrial cancer
C. Myocardial infarction
D. Osteoporosis
E. Stroke
X-66. A 37-year-old man is evaluated for infertility. He and his wife have been attempting to conceive a child for the past 2 years without success. He initially saw an infertility specialist, but was referred to endocrinology after sperm analysis showed no sperm. He is otherwise healthy and only takes a multivitamin. On physical examination his vital signs are normal. He is tall and has small testes, gynecomastia, and minimal facial and axillary hair. Chromosomal analysis confirms Klinefelter’s syndrome. Which of the following statements is true?
A. Androgen supplementation is of little use in this condition.
B. He is not at increased risk for breast tumors.
C. Increased plasma concentrations of estrogen are present.
D. Most cases are diagnosed prepuberty.
E. Plasma concentrations of FSH and LH are decreased in this condition.
X-67. A 17-year-old woman is evaluated in your office for primary amenorrhea. She feels as if she has not entered puberty in that she has never had a menstrual period and has sparse axillary and pubic hair growth. On examination, she is noted to be 150 cm tall. She has a low hairline and slight webbing of her neck. Her follicle-stimulating hormone level is 75 mIU/mL, luteinizing hormone is 20 mIU/mL, and estradiol level is 2 pg/mL. You suspect Turner’s syndrome. All of the following tests are indicated in this individual EXCEPT:
A. Buccal smear for nuclear heterochromatin (Barr body)
B. Echocardiogram
C. Karyotype analysis
D. Renal ultrasound
E. Thyroid-stimulating hormone (TSH)
X-68. A 35-year-old man is seen in the emergency department for evaluation of epigastric pain, diarrhea, and reflux. He reports frequent similar episodes and has undergone multiple endoscopies. In each case he was told that he has a duodenal ulcer. He has become quite frustrated because he was told that ulcers are usually due to a bacteria that can be treated, but he does not have Helicobacter pylori present on any of his ulcer biopsies. His current medications are high-dose omeprazole and oxycodone/acetaminophen. He is admitted to the hospital for pain control. Which of the following is the most appropriate next step in his diagnostic evaluation?
A. CT scan of the abdomen.
B. Discontinue omeprazole for 1 week and measure plasma gastrin level.
C. Gastric pH measurement.
D. Plasma gastrin level.
E. Screen for parathyroid hyperplasia.
X-69. A 48-year-old female is undergoing evaluation for flushing and diarrhea. Physical examination is normal except for nodular hepatomegaly. A CT scan of the abdomen demonstrates multiple nodules in both lobes of the liver consistent with metastases in the liver and a 2-cm mass in the ileum. The 24-hour urinary 5-HIAA excretion is markedly elevated. All the following treatments are appropriate EXCEPT:
A. Diphenhydramine
B. Interferon α
C. Octreotide
D. Ondansetron
E. Phenoxybenzamine
X-70. While undergoing a physical examination during medical student clinical skills, the patient in question X-69 develops severe flushing, wheezing, nausea, and lightheadedness. Vital signs are notable
for a blood pressure of 70/30 mmHg and a heart rate of 135 beats/min. Which of the following is the most appropriate therapy?
A. Albuterol
B. Atropine
C. Epinephrine
D. Hydrocortisone
E. Octreotide
X-71. A 49-year-old male is brought to the hospital by his family because of confusion and dehydration. The family reports that for the last 3 weeks he has had persistent copious, watery diarrhea that has not abated with the use of over-the-counter medications. The diarrhea has been unrelated to food intake and has persisted during fasting. The stool does not appear fatty and is not malodorous. The patient works as an attorney, is a vegetarian, and has not traveled recently. No one in the household has had similar symptoms. Before the onset of diarrhea, he had mild anorexia and a 5-lb weight loss. Since the diarrhea began, he has lost at least 5 kg. The physical examination is notable for blood pressure of 100/70 mmHg, heart rate of 110 beats/min, and temperature of 36.8°C (98.2°F). Other than poor skin turgor, confusion, and diffuse muscle weakness, the physical examination is unremarkable. Laboratory studies are notable for a normal complete blood count and the following chemistry results:
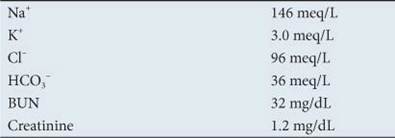
A 24-hour stool collection yields 3 L of tea-colored stool. Stool sodium is 50 meq/L, potassium is 25 meq/L, and stool osmolality is 170 mosmol/L. Which of the following diagnostic tests is most likely to yield the correct diagnosis?
A. Serum cortisol
B. Serum TSH
C. Serum VIP
D. Urinary 5-HIAA
E. Urinary metanephrine
X-72. An 18-year-old girl is evaluated at her primary care physician’s office for a routine physical. She is presently healthy. Her family history is notable for a father and two aunts with MEN 1, and the patient has undergone genetic testing and carries the MEN 1 gene. Which of the following is the first and most common presentation for individuals with this genetic mutation?
A. Peptic ulcer disease
B. Hypercalcemia
C. Hypoglycemia
D. Amenorrhea
E. Uncontrolled systemic hypertension
X-73. A 35-year-old male is referred to your clinic for evaluation of hypercalcemia noted during a health insurance medical screening. He has noted some fatigue, malaise, and a 4-lb weight loss over the last 2 months. He also has noted constipation and “heartburn.” He is occasionally nauseated after large meals and has water brash and a sour taste in his mouth. The patient denies vomiting, dysphagia, or odynophagia. He also notes decreased libido and a depressed mood. Vital signs are unremarkable. Physical examination is notable for a clear oropharynx, no evidence of a thyroid mass, and no lymphadenopathy. Jugular venous pressure is normal. Heart sounds are regular with no murmurs or gallops. The chest is clear. The abdomen is soft with some mild epigastric tenderness. There is no rebound or organomegaly. Stool is guaiac positive. Neurologic examination is nonfocal. Laboratory values are notable for a normal complete blood count. Calcium is 11.2 mg/dL, phosphate is 2.1 mg/dL, and magnesium is 1.8 meq/dL. Albumin is 3.7 g/dL, and total protein is 7.0 g/dL. TSH is 3 μIU/mL, prolactin is 250 μg/L, testosterone is 620 ng/dL, and serum insulin-like growth factor 1 (IGF-1) is normal. Serum intact parathyroid hormone level is 135 pg/dL. In light of the patient’s abdominal discomfort and heme-positive stool, you perform an abdominal computed tomography (CT) scan that shows a lesion measuring 2 × 2 cm in the head of the pancreas. What is the diagnosis?
A. Multiple endocrine neoplasia (MEN) type 1
B. MEN type 2a
C. MEN type 2b
D. Polyglandular autoimmune syndrome
E. Von-Hippel Lindau (VHL) syndrome
X-74. A 55-year-old male is admitted to the intensive care unit with fever and cough. He was well until 1 week before admission, when he noted progressive shortness of breath, cough, and productive sputum. On the day of admission the patient’s wife noted him to be lethargic. Emergency response found the patient unresponsive. He was intubated in the field and brought to the emergency department. His medications include insulin. The past medical history is notable for alcohol abuse and diabetes mellitus. Temperature is 38.9°C (102°F), blood pressure is 76/40 mmHg, and oxygen saturation is 86% on room air. On examination, the patient is intubated on mechanical ventilation. Jugular venous pressure is normal. There are decreased breath sounds at the right lung base with egophony. Heart sounds are normal. The abdomen is soft. There is no peripheral edema. Chest radiography shows a right lower lobe infiltrate with a moderate pleural effusion. An electrocardiogram is normal. Sputum Gram stain shows gram-positive diplococci. White blood cell count is 23 × 103/μL, with 70% polymorphonuclear cells and 6% bands. Blood urea nitrogen is 80 mg/dL, and creatinine is 3.1 mg/dL. Plasma glucose is 425 mg/dL. He is started on broad-spectrum antibiotics, intravenous fluids, omeprazole, and an insulin drip. A nasogastric tube is inserted, and tube feedings are started. On hospital day 2, his creatinine improves to 1.6 mg/dL. However, plasma phosphate is 1.0 mg/dL (0.3 mmol/L) and calcium is 8.8 mg/dL. All of following are causes of hypophosphatemia in this patient EXCEPT:
A. Alcoholism
B. Insulin
C. Malnutrition
D. Renal failure
E. Sepsis
X-75. In the patient in question X-74, what is the most appropriate approach to correcting the hypophosphatemia?
A. Administer IV calcium gluconate 1 g followed by infusion of IV phosphate at a rate of 8 mmol/h
for 6 hours.
B. Administer IV phosphate alone at a rate of 2 mmol/h for 6 hours.
C. Administer IV phosphate alone at a rate of 8 mmol/h for 6 hours.
D. Continue close observation as redistribution of phosphate is expected to normalize over the
course of the next 24–48 hours.
E. Initiate oral phosphate replacement at a dose of 1500 mg/d.
X-76. A 35-year-old woman is admitted to the hospital at 37 weeks’ gestation following a seizure associated with an elevated blood pressure to 190/96 mmHg. She is treated acutely with magnesium sulfate intravenously for eclampsia and is starting on a continuous magnesium sulfate infusion at 1 g/h, which will be continued for 24 hours following her seizure. An emergency caesarian section is planned. Serum magnesium levels will be measured every 6 hours. What magnesium level would be worrisome for the development of central nervous system depression, respiratory muscle paralysis, and cardiac arrhythmias?
A. 0.5 mmol/L
B. 1.0 mmol/L
C. 2.5 mmol/L
D. 3.0 mmol/L
E. 5.0 mmol/L
X-77. You are caring for a 72-year-old man who has been living in a nursing home for the past 3 years. He has severe chronic obstructive pulmonary disease and requires continuous oxygen at 3 L/min. He also previously had a stroke, which has left him with a right hemiparesis. His current medications include aspirin, losartan, hydrochlorothiazide, fluticasone/salmeterol, tiotropium, and albuterol. His body mass index is 18.5 kg/m2. You are concerned that he may have vitamin D deficiency. Which of the following is the best test to determine if vitamin D deficiency is present?
A. 1,25-hydroxy vitamin D
B. 25-hydroxy vitamin D
C. Alkaline phosphatase
D. Parathyroid hormone
E. Serum total and ionized calcium levels
X-78. A 42-year-old man presents to the emergency department with acute-onset right-sided flank pain. He describes the pain as 10 out of 10 in severity radiating to the groin. He has had one episode of hematuria. A noncontrast CT scan confirms the presence of a right-sided renal stone that is currently located in the distal ureter. He has a past medical history of pulmonary sarcoidosis that is not currently treated. This was diagnosed by bronchoscopic biopsy showing noncaseating granulomas. His chest
radiograph shows bilateral hilar adenopathy. His serum calcium level is 12.6 mg/dL. What is the mechanism of hypercalcemia in this patient?
A. Increased activation of 25-hydroxy vitamin D to 1,25-hydroxy vitamin D by macrophages within
granulomas
B. Increased activation of 25-hydroxy vitamin D to 1,25-hydroxy vitamin D by the kidney
C. Increased activation of vitamin D to 25-hydroxy vitamin D by macrophages within granulomas
D. Missed diagnosis of lymphoma with subsequent bone marrow invasion and resorption of bone
through local destruction
E. Production of parathyroid hormone–related peptide by macrophages within granulomas
X-79. A 52-year-old man has end-stage kidney disease from long-standing hypertension and diabetes mellitus. He has been managed with hemodialysis for the past 8 years. Throughout this time, he has been poorly compliant with his medications and hemodialysis schedule, frequently missing one session weekly. He is now complaining of bone pain and dyspnea. His oxygen saturation is noted to be 92% on room air, and his chest radiograph shows hazy bilateral infiltrates. Chest CT shows ground-glass infiltrates bilaterally. His laboratory data include calcium of 12.3 mg/dL, phosphate of 8.1 mg/dL, and parathyroid hormone of 110 pg/mL. Which of the following would be the best approach to the treatment of the patient’s current clinical condition?
A. Calcitriol 0.5 μg intravenously with hemodialysis with sevelamer three times daily
B. Calcitriol 0.5 μg orally daily with sevelamer 1600 mg three times daily
C. More aggressive hemodialysis to achieve optimal fluid and electrolyte balance
D. Parathyroidectomy
E. Sevelamer 1600 mg three times daily
X-80. A 54-year-old woman undergoes total thyroidectomy for follicular carcinoma of the thyroid. About 6 hours after surgery, the patient complains of tingling around her mouth. She subsequently develops a pins-and-needles sensation in the fingers and toes. The nurse calls the physician to the bedside to evaluate the patient after she has severe hand cramps when her blood pressure is taken. Upon evaluation, the patient is still complaining of intermittent cramping of her hands. Since surgery, she has received morphine sulfate 2 mg for pain and Compazine 5 mg for nausea. She has had no change in her vital signs and is afebrile. Tapping on the inferior portion of the zygomatic arch 2 cm anterior to the ear produces twitching at the corner of the mouth. An electrocardiogram (ECG) shows a QT interval of 575 milliseconds. What is the next step in the evaluation and treatment of this patient?
A. Administration of benztropine 2 mg IV
B. Administration of calcium gluconate 2 g IV
C. Administration of magnesium sulphate 4 g IV
D. Measurement of calcium, magnesium, phosphate, and potassium levels
E. Measurement of forced vital capacity
X-81. A 68-year-old woman with stage IIIB squamous cell carcinoma of the lung is admitted to the hospital because of altered mental status and dehydration. Upon admission, she is found to have a calcium level of 19.6 mg/dL and phosphate of 1.8 mg/dL. Concomitant measurement of parathyroid hormone was 0.1 pg/mL (normal 10–65 pg/mL), and a screen for parathyroid hormone–related peptide
was positive. Over the first 24 hours, the patient receives 4 L of normal saline with furosemide diuresis. The next morning, the patient’s calcium is 17.6 mg/dL and phosphate is 2.2 mg/dL. She continues to have delirium. What is the best approach for ongoing treatment of this patient’s hypercalcemia?
A. Continue therapy with large-volume fluid administration and forced diuresis with furosemide.
B. Continue therapy with large-volume fluid administration, but stop furosemide and treat with
hydrochlorothiazide.
C. Initiate therapy with calcitonin alone.
D. Initiate therapy with pamidronate alone.
E. Initiate therapy with calcitonin and pamidronate.
X-82. A 60-year-old woman is referred to your office for evaluation of hypercalcemia of 12.9 mg/dL. This was found incidentally on a chemistry panel that was drawn during a hospitalization for cervical spondylosis. Despite fluid administration in the hospital, her serum calcium at discharge was 11.8 mg/dL. The patient is asymptomatic. She is otherwise in good health and has had her recommended age-appropriate cancer screening. She denies constipation or bone pain and is now 8 weeks out from her spinal surgery. Today, her serum calcium level is 12.4 mg/dL, and phosphate is 2.3 mg/dL. Her hematocrit and all other chemistries including creatinine were normal. What is the most likely diagnosis?
A. Breast cancer
B. Hyperparathyroidism
C. Hyperthyroidism
D. Multiple myeloma
E. Vitamin D intoxication
X-83. All of the following are actions of parathyroid hormone EXCEPT:
A. Direct stimulation of osteoblasts to increase bone formation
B. Direct stimulation of osteoclasts to increase bone resorption
C. Increased reabsorption of calcium from the distal tubule of the kidney
D. Inhibition of phosphate reabsorption in the proximal tubule of the kidney
E. Stimulation of renal 1-α-hydroxylase to produce 1,25-hydroxycholecalciferol
X-84. Which of the following statements regarding the epidemiology of osteoporosis and bone fractures is correct?
A. For every 5-year period after age 70, the incidence of hip fractures increases by 25%.
B. Fractures of the distal radius increase in frequency before age 50 and plateau by age 60 with
only a modest age-related increase.
C. Most women meet the diagnostic criteria for osteoporosis between the ages of 60 and 70.
D. The risk of hip fracture is equal when white women are compared to black women.
E. Women outnumber men with osteoporosis at a ratio of about 10 to 1.
X-85. A 50-year-old woman presents to your office to inquire about her risk of fracture related to
osteoporosis. She has a positive family history of osteoporosis in her mother, but her mother never experienced any hip or vertebral fractures. The patient herself has also not experienced any fractures. She is white and has a 20 pack-year history of tobacco, quitting 10 years prior. At the age of 37, she had a total hysterectomy with bilateral salpingo-oophorectomy for endometriosis. She is lactose intolerant and does not consume dairy products. She currently takes calcium carbonate 500 mg daily. Her weight is 52 kg. All of the following are risk factors for an osteoporotic fracture in this woman EXCEPT:
A. Early menopause
B. Female sex
C. History of cigarette smoking
D. Low body weight
E. Low calcium intake
X-86. All of the following diseases are associated with an increased risk of osteoporosis EXCEPT:
A. Anorexia nervosa
B. Chronic obstructive pulmonary disease
C. Congestive heart failure
D. Malabsorption syndromes
E. Hyperparathyroidism
X-87. A 54-year-old woman is referred to the endocrinology clinic for evaluation of osteoporosis after a recent examination for back pain revealed a compression fracture of the T4 vertebral body. She is
perimenopausal with irregular menstrual periods and frequent hot flashes. She does not smoke. She otherwise is well and healthy. Her weight is 70 kg and height is 168 cm. She has lost 5 cm from her maximum height. A bone mineral density scan shows a T-score of –3.5 SD and a Z-score of –2.5 SD. All of the following tests are indicated for the evaluation of osteoporosis in this patient EXCEPT:
A. 24-hour urine calcium
B. Follicle-stimulating hormone and luteinizing hormone levels
C. Serum calcium
D. Thyroid-stimulating hormone
E. Vitamin D levels (25-hydroxyvitamin D)
X-88. A 45-year-old white woman seeks advice from her primary care physician regarding her risk for osteoporosis and the need for bone density screening. She is a lifelong nonsmoker and drinks alcohol only socially. She has a history of moderate-persistent asthma since age 12. She is currently on fluticasone, 44 mg/puff twice daily, with good control currently. She last required oral prednisone therapy about 6 months ago when she had influenza that was complicated by an asthma flare. She took prednisone for a total of 14 days. She has had three pregnancies and two live births at ages 39 and 41. She currently has irregular periods occurring approximately every 42 days. Her follicle-stimulating hormone level is 25 mIU/L and 17β-estradiol level is 115 pg/mL on day 12 of her menstrual cycle. Her mother and maternal aunt both have been diagnosed with osteoporosis. Her mother also has rheumatoid arthritis and requires prednisone therapy, 5 mg daily. Her mother developed a compression fracture of the lumbar spine at age 68. On physical examination, the patient appears well and healthy. Her height is
168 cm. Her weight is 66.4 kg. The chest, cardiac, abdominal, muscular, and neurologic examinations are normal. What do you tell the patient about the need for bone density screening?
A. As she is currently perimenopausal, she should have a bone density screen every other year until
she completes menopause and then have bone densitometry measured yearly thereafter.
B. Because of her family history, she should initiate bone density screening yearly beginning now.
C. Bone densitometry screening is not recommended until after completion of menopause.
D. Delayed childbearing until the fourth and fifth decade decreases her risk of developing
osteoporosis so bone densitometry is not recommended.
E. Her use of low-dose inhaled glucocorticoids increases her risk of osteoporosis threefold, and
she should undergo yearly bone density screening.
X-89. What is the definition of osteoporosis by dual-energy x-ray absorptiometry testing (bone densitometry)?
Date: 2016-04-22; view: 823