
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
TABLE IV-114 Risk Factors for Active Tuberculosis Among Persons Who Have Been Infected With Tubercle Bacilli 8 page
A. Atrial premature contractions are less common than ventricular premature contractions on
extended ECG monitoring.
B. Echocardiography is indicated to determine if structural heart disease is present.
C. Metoprolol should be initiated for symptom control.
D. The patient should be reassured that this is not a dangerous condition and does not require
further evaluation.
E. The patient should undergo a stress test to determine if ischemia is present.
V-28. A 55-year-old man with end-stage COPD is admitted to the intensive care unit with an exacerbation of his obstructive lung disease. Because of hypercarbic respiratory failure, he is intubated and placed on assist-control mechanical ventilation. Despite aggressive sedation, his ventilator alarms several times that peak inspiratory pressures are high. The physician is called to the bedside to evaluate tachycardia. Examination is notable for a blood pressure of 112/68 mmHg and heart rate of 180 beats/min. Cardiac examination shows a regular rhythm, but no other abnormality. Breath sounds are decreased on the right. ECG shows narrow complex tachycardia. With carotid sinus massage, the heart rate transiently drops to 130 beats/min, but then returns to 180 beats/min. Which of the following is the most appropriate next step in management?
A. Adenosine 25-mg IV push
B. Amiodarone 200-mg IV push
C. Chest radiograph
D. Metoprolol 5-mg IV push
E. Sedation followed by cardioversion
V-29. All of the following are risk factors for stroke in a patient with atrial fibrillation EXCEPT:
A. Diabetes mellitus
B. History of congestive heart failure
C. History of stroke
D. Hypertension
E. Left atrial size greater than 4.0 cm
V-30. Which of the following statements regarding restoration of sinus rhythm after atrial fibrillation is true?
A. Dofetilide may be safely started on an outpatient basis.
B. In patients who are treated with pharmacotherapy and are found to be in sinus rhythm, a
prolonged Holter monitor should be worn to determine if anticoagulation could be safely stopped.
C. Patients who have pharmacologically maintained sinus rhythm after atrial fibrillation have
improved survival compared with patients who are treated with rate control and anticoagulation.
D. Recurrence of atrial fibrillation is uncommon when pharmacotherapy is used to maintain sinus
rhythm.
V-31. A 57-year-old woman with a history of a surgically corrected atrial septal defect in childhood presents to the emergency department with palpitations for 3 days. She is found to have a heart rate of 153 beats/min and blood pressure of 128/75 mmHg, and an ECG shows atrial flutter. An echocardiogram demonstrates moderate right and left atrial dilation, postoperative changes from her surgery, and normal left and right ventricular function. Which of the following is true?
A. Anticoagulation with dabigatran should be initiated.
B. If a transesophageal echocardiogram does not demonstrate left atrial thrombus, she may be
cardioverted without anticoagulation.
C. Intravenous heparin should be started immediately.
D. She should be immediately cardioverted.
E. Transthoracic echocardiogram is adequate to rule out the presence of left atrial thrombus.
V-32. A patient presents with palpitations and shortness of breath for 6 hours. In the emergency department waiting room an ECG is performed (shown in Figure V-32). Which of the following is most likely to be found on physical examination?
A. Diffuse abdominal tenderness with guarding
B. Diffuse expiratory polyphonic wheezing with poor air movement and hyperinflation
C. Left ventricular heave and third heart sound
D. Supraclavicular lymphadenopathy
E. Vesicular rash over right T5 dermatome
HI
Í

FIGURE V-32
V-33. A 43-year-old woman is seen in the emergency department after sudden onset of palpitations 30 minutes prior to her visit. She was seated at her work computer when the symptoms began. Aside from low back pain, she is otherwise healthy. In triage, her heart rate is 178 beats/min, and blood pressure is 98/56 mmHg with normal oxygen saturation. On physical examination, she has a “frog sign” in her neck and tachycardia, but is otherwise normal. ECG shows a narrow complex tachycardia without identifiable P waves. Which of the following is the most appropriate first step to manage her tachycardia?
A. 5 mg metoprolol IV
B. 6 mg adenosine IV
C. 10 mg verapamil IV
D. Carotid sinus massage
E. DC cardioversion using 100 J
V-34. A 37-year-old man who is healthy aside from a prior knee surgery is evaluated in the emergency department for palpitations that developed suddenly while eating dinner. He is found to have a heart rate of 193 beats/min, blood pressure of 92/52 mmHg, and normal oxygen saturation. His physical examination is normal aside from tachycardia and mild diaphoresis. An ECG obtained before his knee surgery shows delta waves in the early precordial leads. His current ECG shows wide complex tachycardia. Which of the following therapies is contraindicated for treatment of his tachyarrhythmia?
A. Adenosine
B. Carotid sinus massage
C. DC cardioversion
D. Digoxin
E. Metoprolol
V-35. In an ECG with wide complex tachycardia, which of the following clues most strongly supports the diagnosis of ventricular tachycardia?
A. Atrial-ventricular dissociation
B. Classic right bundle branch block pattern
C. Irregularly irregular rhythm with changing QRS complexes
D. QRS duration greater than 120 milliseconds
E. Slowing of rate with carotid sinus massage
V-36. A 40-year-old male with diabetes and schizophrenia is started on antibiotic therapy for chronic osteomyelitis in the hospital. His osteomyelitis has developed just under an ulcer where he has been injecting heroin. He is found suddenly unresponsive by the nursing staff. His electrocardiogram is shown in Figure V-36. The most likely cause of this rhythm is which of the following substances?
A. Furosemide
B. Metronidazole
C. Droperidol
D. E.
Metformin Heroin
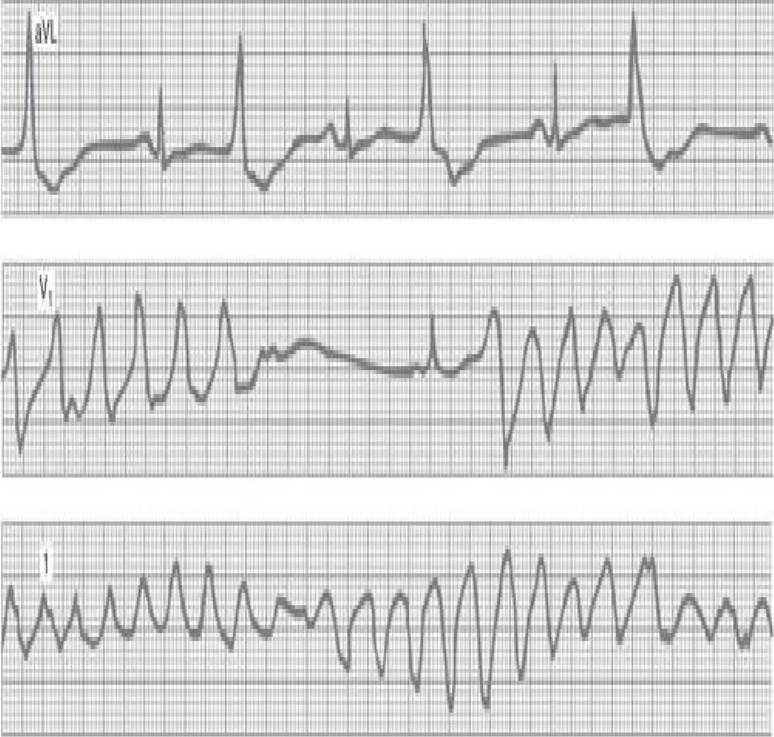
FIGURE V-36
V-37. Normal sinus rhythm is restored with electrical cardioversion in the patient in question V-36. A 12-lead electrocardiogram is notable for a prolonged QT interval. Besides stopping the offending drug, the most appropriate management for this rhythm disturbance should include intravenous administration of which of the following?
A. Amiodarone
B. Lidocaine
C. Magnesium
D. Metoprolol
E. Potassium
V-38. You are caring for a patient with heart rate–related angina. With minor elevations in heart rate, the patient has anginal symptoms that impact his quality of life. On review of a 24-hour Holter monitor, it appears that the patient has sinus tachycardia at the time of his symptoms. What is the mechanism for this patient’s arrhythmia?
A. Delayed afterdepolarizations
B. Early afterdepolarizations
C. Increased automaticity
D. Reentry pathway
V-39. Where are the most common drivers of atrial fibrillation anatomically located?
A. Left atrial appendage
B. Mitral annulus
C. Pulmonary vein orifice
D. Sinus venosus
E. Sinus node
V-40. Symptoms of atrial fibrillation vary dramatically from patient to patient. A patient with which of the following clinical conditions will likely be the most symptomatic (e.g., short of breath) if the patient develops atrial fibrillation?
A. Acute alcohol intoxication
B. Hypertrophic cardiomyopathy
C. Hyperthyroidism
D. Hypothermia
E. Postoperative after thoracotomy
V-41. A 47-year-old postmenopausal woman is seen for onset of severe dyspnea over the last few weeks. She reports no preceding chest pain, cough, sputum, or fever, though she does report leg swelling. Physical examination is notable for a blood pressure of 145/78 mmHg and heart rate of 123 beats/min. Exophthalmos is present as well as bilateral inspiratory crackles occupying approximately one-third of the lower chest; neck vein distention; normal cardiac rhythm, though tachycardia is present; and a third heart sound with no murmur. Bilateral lower extremity edema and a fine hand tremor are also present. Which of the following is the most likely pathophysiologic explanation for her heart failure?
A. Anemia with high-output state
B. Chronic systemic hypertension with resultant left ventricular hypertrophy and nonsystolic heart
failure
C. Hemochromatosis with subsequent restrictive cardiomyopathy
D. Myocardial infarction with depressed left ventricular systolic function
E. Thyrotoxicosis with high-output state
V-42. Which of the following statements is true regarding measurement of plasma BNP to diagnose heart failure?
A. An elevated plasma BNP in a dyspneic patient confirms the diagnosis of left heart failure.
B. In the presence of renal failure, BNP levels are suppressed even when heart failure is present.
C. Plasma BNP levels may be falsely low in patients with obesity and heart failure.
D. Serial measurement of BNP in the therapy of decompensated heart failure should be used to
guide therapy.
E. All of the above are true.
V-43. A 64-year-old man with an ischemic cardiomyopathy, ejection fraction 35%, and stage C heart failure is seen in the cardiology clinic for evaluation of his disease status. The patient reports a regular exercise regimen of walking on the treadmill several times weekly and occasional exacerbations of his leg edema that he manages with an extra dose of furosemide. He has never been hospitalized for heart failure. His current medical regimen includes lisinopril, aspirin, furosemide, atorvastatin, digoxin, spironolactone, and metoprolol. He is interested in stopping medications because of their expense. Which of the following statements is true regarding his medical regimen?
A. ACE inhibition therapy has not been shown to improve heart failure symptoms.
B. Beta blocker therapy in this patient may be exacerbating his occasional need for extra
furosemide and therefore should be stopped.
C. He should be switched from spironolactone to eplerenone for improved efficacy, as seen in
patients with EF less than 35%.
D. If digoxin is withdrawn, he will likely have worsening symptoms.
E. If he is intolerant to lisinopril because of cough, it would be reasonable to switch him to an
angiotensin-receptor blocker.
V-44. A 78-year-old slender woman is seen in the emergency department after several weeks of dyspnea on exertion that progressed to dyspnea at rest following a summer cookout where she consumed multiple pickled vegetables. She also complains of leg swelling, orthopnea, and occasionally awakening at night with dyspnea. Her past medical history is notable for long-standing systemic hypertension, uterine prolapse, and an anxiety disorder. Examination confirms the presence of heart failure with a laterally displaced and sustained point of maximum impulse and a fourth heart sound. She is admitted to the hospital and given diuretics, and an echocardiogram is obtained. Echocardiography reveals severe left ventricular hypertrophy with an ejection fraction of 70%, but there are no focal wall motion abnormalities, and aortic and mitral valvular function is intact. Her right ventricular systolic pressure is estimated to be 45 mmHg. After resolution of her heart failure symptoms with diuresis, the patient is ready for discharge. Which of the following medications have been shown to improve mortality in patients with heart failure with preserved ejection fraction and should be included in this patient’s regimen?
A. Digoxin
B. Lisinopril
C. Metoprolol
D. Sildenafil
E. None of the above
V-45. A 68-year-old man with a history of myocardial infarction and congestive heart failure is comfortable at rest. However, when walking to his car he develops dyspnea, fatigue, and sometimes palpitations. He must rest for several minutes before these symptoms resolve. His New York Heart Association classification is which of the following?
A. Class I
B. Class II
C. Class III
D. Class IV
V-46. The husband of a 68-year-old woman with congestive heart failure is concerned because his wife appears to stop breathing for periods of time when she sleeps. He has noticed that she stops breathing for approximately 10 seconds and then follows this with a similar period of hyperventilation. This does not wake her from sleep. She does not snore. She feels well rested in the morning but is very dyspneic with even mild activity. What is your next step in management?
A. Electroencephalography
B. Maximize heart failure management
C. Nasal continuous positive airway pressure (CPAP) during sleep
D. Obtain a sleep study
E. Prescribe bronchodilators
V-47. A 53-year-old man undergoes cardiac transplantation for end-stage ischemic cardiomyopathy due to an underlying familial hypercholesterolemic disorder. His donor was a 23-year-old motor vehicle accident victim. The patient does well for the first 3 years after transplantation with only a single episode of acute rejection. He shows good compliance with his immunosuppression regimen, which includes prednisone and sirolimus. He is evaluated at a routine follow-up visit and reports that he has developed dyspnea on exertion. His pulmonary function tests are unchanged and a chest radiograph is normal. He undergoes right and left heart catheterization with biopsy of the transplanted heart. Severe, diffuse, concentric, and longitudinal coronary artery disease is found on coronary angiography, and histology shows no evidence of acute rejection. Which of the following statements is true regarding the coronary atherosclerosis found in this patient?
A. No immunosuppressive regimen has been shown to have a lower incidence of coronary
atherosclerosis after cardiac transplantation.
B. The coronary atherosclerosis is most likely immunologic injury of the vascular endothelium in
the transplanted organ.
C. The current coronary atherosclerosis after cardiac transplant is likely due to atherosclerosis
present prior to transplantation.
D. The patient’s underlying cholesterol disorder did not predispose him to recurrent coronary
atherosclerosis after cardiac transplantation.
E. Therapy with statins has not been associated with a reduced incidence of this complication of
transplantation.
V-48. Which of the following is a known complication of ventricular assist device placement in patients with end-stage heart failure?
A. Cerebrovascular accident
B. Infection of insertion site
C. Mechanical device failure
D. Thromboembolism
E. All of the above
V-49. All of the following are potential complications of an atrial septal defect in adults EXCEPT:
A. Air embolism from a central venous catheter
B. Arterial oxygen desaturation with exertion
C. Embolic cerebrovascular accident
D. Pulmonary arterial hypertension
E. Unstable angina
V-50. A 32-year-old woman is seen by her primary care physician clinic for routine follow-up of her hypothyroidism. She also has a history of complex congenital heart disease with a partially corrected VSD with predominantly right to left shunt across her patch. She is doing well and is able to work in janitorial services without severe dyspnea. She denies any heart failure or neurologic symptoms, but does have a peripheral oxygen saturation of 78%. A routine CBC is drawn and shows a hematocrit of 65%. Which of the following is the most appropriate management of her elevated hematocrit?
A. Begin oxygen therapy
B. Check co-oximetry on arterial blood gas sample
C. Check serum erythropoietin level
D. Expectant waiting
E. Refer to hematology for phlebotomy
V-51. A 43-year-old man recently was found to have an asymptomatic atrial septal defect that was closed using a percutaneous patch 1 month ago without complication. He is undergoing a root canal at the dentist next week and calls his primary care office to determine if antibiotic prophylaxis is indicated. Which of the following statements is true regarding antibiotic prophylaxis in this patient?
A. Because he had only simple congenital heart disease, no prophylaxis is indicated.
B. Because the lesion is corrected, no prophylaxis is indicated.
C. He should avoid potentially bacteremic dental procedures unless no other alternative is
available.
D. Routine antibiotic prophylaxis is indicated for bacteremic dental procedures, particularly if the
patch is less than 6 months old.
E. Routine antibiotic prophylaxis is indicated for bacteremic dental procedures whenever foreign
material is present.
V-52. A 20-year-old man undergoes a physical examination with chest radiograph for enrollment in the military. He has had a normal childhood without any major illness. There is no history of sinusitis,
pneumonia, or chronic respiratory disease. Chest radiograph shows dextrocardia. On closer physical examination, a spleen tip is palpable on the right of the abdomen and the liver can be percussed on the left. Which of the following is true regarding his condition?
A. He is likely to have aortic stenosis.
B. He is likely to have aspermia.
C. He is likely to have an atrial septal defect.
D. He is likely to have a ventriculoseptal defect.
E. He is likely to otherwise be normal.
V-53. A 24-year-old male seeks medical attention for the recent onset of headaches. The headaches are described as “pounding” and occur during the day and night. He has had minimal relief with acetaminophen. Physical examination is notable for a blood pressure of 185/115 mmHg in the right arm, a heart rate of 70 beats/min, arterioventricular (AV) nicking on funduscopic examination, normal jugular veins and carotid arteries, a pressure-loaded PMI with an apical S4, no abdominal bruits, and
reduced pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. Additional measurement of blood pressure reveals the following:
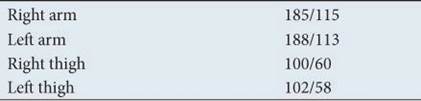
Which of the following diagnostic studies is most likely to demonstrate the cause of the headaches?
A. MRI of the head
B. MRI of the kidney
C. MRI of the thorax
D. 24-hour urinary 5-HIAA
E. 24-hour urinary free cortisol
V-54. The patient described in question V-53 is most likely to have which of the following associated cardiac abnormalities?
A. Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. Right bundle branch block
E. Tricuspid atresia
V-55. Mitral stenosis is frequently complicated by pulmonary hypertension. Which of the following is a cause of pulmonary hypertension in mitral stenosis?
A. Interstitial edema in the walls of small pulmonary vessels
B. Passive transmission of elevated left atrial pressure
C. Obliterative changes in the pulmonary vascular bed
D. Pulmonary arteriolar constriction
E. All of the above
V-56. A 58-year-old man with a history of systemic hypertension, hyperlipidemia, and tobacco abuse is admitted to the intensive care unit with crushing chest pain associated with ST-segment elevation and small precordial Q waves. Because his symptoms have been present for 36 hours, he is not a candidate for thrombolytics. On admission to the ICU, his systemic blood pressure is 123/67 mmHg, heart rate is 67 beats/min after beta blockade, and his oxygenation saturation is 93% on 2L nasal cannula. The remainder of the physical examination is normal. He is treated with lisinopril, aspirin, heparin, and metoprolol. Before transfer can be arranged to a tertiary center, the patient reports extreme dyspnea. He is found to be diaphoretic and to have a heart rate of 80 beats/min, blood pressure of 84/56 mmHg, and oxygen saturation of 93% on 100% non-rebreather. His lungs have bilateral crackles throughout, and neck veins are moderately elevated. ECG is unchanged. Chest radiograph shows new alveolar infiltrates in the right lung greater than the left. Which of the following is a likely finding on physical examination?
A. A fourth heart sound, III/VI systolic murmur heard best at the apex with a “cooing” quality that
radiates to the axilla
B. A right ventricular heave, loud second heart sound, III/VI murmur increasing with inspiration at
the right lower sternal border
C. A third heart sound, III/VI crescendo-decrescendo murmur heard best at the right upper sternal
border
D. Diffuse urticarial reaction, wheezing on pulmonary examination
E. Mucosal edema, finger swelling, stridor
V-57. Which of the following is the most appropriate next step in therapy for the patient in question V-56?
A. Aerosolized albuterol
B. Initiation of norepinephrine infusion
C. Intravenous infusion of nitroprusside
D. Intravenous methylprednisolone
E. Placement of intraaortic balloon pump
V-58. A 26-year-old healthy woman is seen for a pap smear at a routine office visit. She feels well and has no complaints and no significant past medical history. Her internist performs a full physical examination and a midsystolic click is heard. No murmur or gallop is present. She is concerned about this finding. Which of the following statements is true regarding her examination finding?
A. In most patients with this disorder, an underlying cause such as a heritable disorder of
connective tissue is found.
B. Infective endocarditis prophylaxis is indicated for dental procedures potentially associated with
bacteremia.
C. Most patients are asymptomatic from this lesion and will remain so their entire life.
D. She should begin therapy with aspirin 325 mg po daily.
E. This disorder cannot be visualized on echo-cardiography.
V-59. A 78-year-old man is evaluated for the onset of dyspnea on exertion. He has a long history of tobacco abuse, obesity, and diabetes mellitus. His current medications include metformin, aspirin, and occasional ibuprofen. On physical examination his peripheral pulses show a delayed peak and he has a prominent left ventricular heave. He is in a regular rhythm with a IV/VI midsystolic murmur that is loudest at the base of the heart and radiates to the carotid arteries. A fourth heart sound is present. Echocardiography confirms severe aortic stenosis without other valvular lesions. Which of the following most likely contributed to the development of his cardiac lesion?
A. Congenital bicuspid aortic valve
B. Diabetes mellitus
C. Occult rheumatic heart disease
D. Underlying connective tissue disease
E. None of the above
V-60. A 63-year-old man presents with new-onset exertional syncope and is found to have aortic stenosis. In counseling the patient, you tell him that your therapeutic recommendation is based on the observation that untreated patients with his presentation have a predicted average lifespan of:
A. 5 years
B. 4 years
C. 3 years
D. 2 years
E. 1 year
V-61. Which of the following physical examination findings suggests severe aortic regurgitation?
A. Corrigan’s pulse
B. Pulsus alternans
C. Pulsus bigeminus
D. Pulsus paradoxus
E. Pulsus parvus et tardus
V-62. A 41-year-old Somali woman is seen in clinic for onset of hemoptysis in the sixth month of her pregnancy. This is her fourth pregnancy and the others were uncomplicated, though she was 35 years old at the birth of her last child. Prior to this, she had been healthy. She reports mild dyspnea beginning at the fourth month of her pregnancy with onset of mild leg swelling shortly thereafter that she attributed to her pregnancy. The dyspnea has become severe, and she is now limited to walking around her house. She began to cough small amounts of bloody sputum 5 days ago. She had neither fever nor purulent sputum and has not responded to a course of antibiotics prescribed by her obstetrician. Physical examination is notable for a normal temperature, heart rate of 110 beats/min, blood pressure of 108/60 mmHg, and oxygen saturation of 91% on room air. No source of bleeding is seen in her nares or oropharynx. Her lungs have diffuse crackles, and cardiac examination shows moderately elevated neck veins, a regular heart rhythm, a loud second heart sound, and a low-pitched diastolic rumble heard best at the apex. The abdomen has a gravid uterus, and 1+ lower extremity edema is present. Which of the following is most likely to demonstrate the cause of her symptoms?
A. Bronchoscopy
B. Chest CT with contrast
C. Echocardiogram
D. Right heart catheterization
E. Upper airway inspection by an otolaryngologist
V-63. In the patient described in question V-62, which of the following should be prescribed at her visit to alleviate her symptoms?
A. Benazepril
B. Digoxin
C. Furosemide
D. Heparin
E. Levofloxacin
V-64. Which of the following patients with echocardiographic evidence of significant mitral regurgitation has the best indication for surgery with the most favorable likelihood of a positive outcome?
A. A 52-year-old man with an ejection fraction of 25%, NYHA class III symptoms, and a left-
ventricular end-systolic dimension of 60 mm
B. A 54-year-old man with an ejection fraction of 30%, NYHA class II symptoms, and pulmonary
hypertension
C. A 63-year-old man in sinus rhythm without symptoms, an ejection fraction of 65%, and a normal
right heart catheterization
D. A 66-year-old man without symptoms, an ejection fraction of 50%, and left-ventricular end-
systolic dimension of 45 mm
E. A 72-year-old asymptomatic woman with newly discovered atrial fibrillation, ejection fraction
of 60%, and end-systolic dimension of 35 mm
V-65. All of the following are potential causes of tricuspid regurgitation EXCEPT:
A. Congenital heart disease
B. Infective endocarditis
C. Inferior wall myocardial infarction
D. Pulmonary arterial hypertension
E. Rheumatic heart disease
F. All of the above will cause tricuspid regurgitation.
V-66. All the following are true about cardiac valve replacement EXCEPT:
A. Bioprosthetic valve replacement is preferred to mechanical valve replacement in younger
patients because of the superior durability of the valve.
B. Bioprosthetic valves have a low incidence of thromboembolic complications.
C. The risk of thrombosis with mechanical valve replacement is higher in the mitral position than in
the aortic position.
D. Mechanical valves are relatively contraindicated in patients who wish to become pregnant.
E. Double-disk tilting mechanical prosthetic valves offer superior hemodynamic characteristics over single-disk tilting valves.
V-67. Which of the following infectious agents have been associated with the development of inflammatory myocarditis?
A. Coxsackie virus
B. Diphtheria
C. Q fever
D. Trypanosoma cruzi
E. All of the above
V-68. All of the following are risk factors for the development of peripartum cardiomyopathy EXCEPT:
A. Advanced maternal age
B. Malnutrition
C. Primiparity
D. Twin pregnancy
E. Use of tocolytics
V-69. A 67-year-old man with a long history of alcohol abuse presents with findings consistent with left ventricular failure including pulmonary edema and congestion. He undergoes right heart catheterization and left heart catheterization. No significant coronary artery disease is found. Which of the following right heart catheterization numbers (see Table V-69 ) would support a diagnosis of beriberi heart disease?
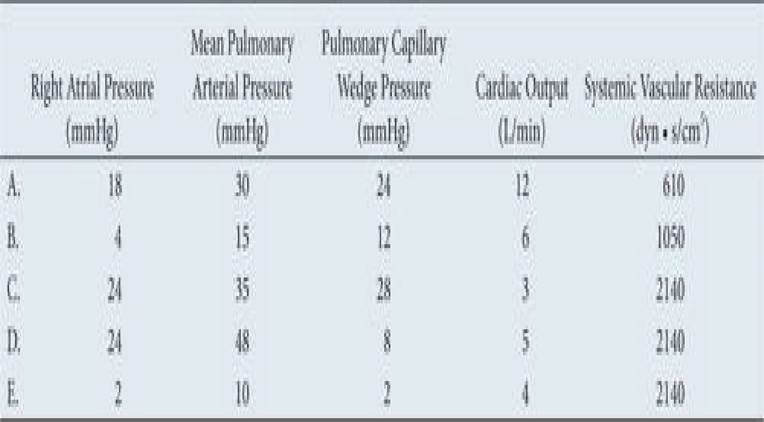
TABLE V-69
V-70. A 20-year-old basketball player is seen for evaluation prior to beginning another season of competitive sports. A harsh systolic murmur is heard at the left lower sternal border. Which of the following maneuvers will enhance this murmur if hypertrophic cardiomyopathy is the underlying cause?
Date: 2016-04-22; view: 1271