
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
ÀÌìÉÀæDVT, Jeep venous [Û)ÛêÐÅ, pulmonary embolism. 6 page
FIGURE IV-198 (see Color Atas)
A. Branching (45°) septated hyphae on methenamine silver stain
B. Budding yeast on methenamine silver stain
C. Encapsulated yeast on India ink stain
D. Pseudohyphae and hyphae on tissue Gram stain
E. Rounded internally septated spherules on methenamine silver stain
IV-199. In the patient described above, all of the following medications are appropriate additions to the current antibiotic regimen EXCEPT:
A. Amphotericin
B. Caspofungin
C. Fluconazole
D. Flucytosine
E. Voriconazole
IV-200. Which of the following statements regarding the use of antifungal agents to prevent Candida infections is true?
A. HIV-infected patients should receive prophylaxis for oropharyngeal candidiasis when CD4
count is below 200 cells/mm3.
B. Most centers administer fluconazole to recipients of allogeneic stem cell transplants.
C. Most centers administer fluconazole to recipients of living related renal transplants.
D. Voriconazole has been shown to be superior to other agents as prophylaxis in liver transplant
recipients.
E. Widespread candida prophylaxis in postoperative patients in the SICU has been shown to be
cost effective.
IV-201. Candida albicans is isolated from the following patients. Rate the likelihood in order from greatest to least that the positive culture represents true infection rather than contaminant or noninfectious colonization.
Patient X: A 63-year-old man admitted to the intensive care unit (ICU) with pneumonia who has recurrent fevers after receiving 5 days of levofloxacin for pneumonia. A urinalysis drawn from a Foley
catheter shows positive leukocyte esterase, negative nitrite, 15 white blood cells/hpf, 10 red blood
cells/hpf, and 10 epithelial cells/hpf. Urine culture grows Candida albicans.
Patient Y: A 38-year-old woman on hemodialysis presents with low-grade fevers and malaise.
Peripheral blood cultures grow C. albicans in one of a total of three sets of blood cultures in the
aerobic bottle only.
Patient Z: A 68-year-old man presents with a 2-day history of fever, productive cough, and malaise.
Chest radiography reveals a left lower lobe infiltrate. A sputum Gram stain shows many PMNs, few
epithelial cells, moderate gram-positive cocci in chains, and yeast consistent with Candida spp.
A. Patient X > patient Z > patient Y
B. Patient Y > patient Z > patient X
C. Patient Y > patient X > patient Z
D. Patient X > patient Y > patient Z
E. Patient Z > patient X > patient Y
IV-202. A 72-year-old man is admitted to the hospital with bacteremia and pyelonephritis. He is HIV-negative and has no other significant past medical history. Two weeks into his treatment with antibiotics, a fever evaluation reveals a blood culture positive for Candida albicans. Examination is unremarkable. White blood cell count is normal. The central venous catheter is removed, and systemic antifungal agents are initiated. What further evaluation is recommended?
A. Abdominal CT scan to evaluate for abscess
B. Chest radiography
C. Funduscopic examination
D. Repeat blood cultures
E. Transthoracic echocardiography
IV-203. A local oncology center is concerned about the occurrence of an outbreak of cases of invasive Aspergillus in patients receiving bone marrow transplants. Which of the following is the most likely source of Aspergillus infection?
A. Contaminated air source
B. Contaminated water source
C. Patient-to-patient spread in outpatient clinic waiting rooms
D. Provider-to-patient spread because of poor hand washing technique
E. Provider-to-patient spread because of poor utilization of alcohol disinfectant
IV-204. A 23-year-old man receiving chemotherapy for relapsed acute myelogenous leukemia has had persistent neutropenia for the past 4 weeks. Over the past 5 days, his absolute neutrophil count has risen from zero to 200 cells/mm3, and he has had persistent fevers despite receiving cefepime and vancomycin empiric therapy. Other than fever, tachycardia, and malaise, he has no focal findings, and his vital signs are otherwise unremarkable, including a normal oxygen saturation on room air. A chest and abdomen CT performed because of the fever shows a few scattered 1- to 2-cm nodules with surrounding ground glass infiltrates in the lower lobes. Which of the following test results will most likely be positive in this patient?
A. Serum cryptococcal antigen
B. Serum galactomannan assay
C. Sputum fungal culture
D. Urine Histoplasma antigen
E. Urine Legionella antigen
IV-205. In the patient described above, which of the following medications should be initiated immediately?
A. Amphotericin B
B. Caspofungin
C. Fluconazole
D. Trimethoprim–sulfamethoxazole
E. Voriconazole
IV-206. A 40-year-old male smoker with a history of asthma is admitted to the inpatient medical service with fever, cough, brownish-green sputum, and malaise. Physical examination shows a respiratory rate of 15 breaths/min, no use of accessory muscles of breathing, and bilateral polyphonic wheezes throughout the lung fields. There is no clubbing or skin lesions. You consider a diagnosis of allergic bronchopulmonary aspergillosis. All the following clinical features are consistent with allergic broncho-pulmonary aspergillosis EXCEPT:
A. Bilateral peripheral cavitary lung infiltrates
B. Elevated serum IgE
C. Peripheral eosinophilia
D. Positive serum antibodies to Aspergillus spp.
E. Positive skin testing for Aspergillus spp.
IV-207. A 26-year-old patient with asthma continues to have coughing fits and dyspnea despite numerous steroid tapers and frequent use of albuterol over the past few months. Persistent infiltrates are seen on chest radiography. A pulmonary consultation suggests an evaluation for allergic bronchopulmonary aspergillosis. Which of the following is the best diagnostic test for this diagnosis?
A. Bronchoalveolar lavage (BAL) with fungal culture
B. Galactomannan enzyme immunoassay (EIA)
C. High-resolution CT
D. Pulmonary function tests
E. Serum IgE level
IV-208. Patients with which of the following have the lowest risk of invasive pulmonary Aspergillus infection?
A. Allogeneic stem cell transplant with graft-versus-host disease
B. HIV infection
C. Long-standing high-dose glucocorticoids
D. Post-solid organ transplant with multiple episodes of rejection
E. Relapsed or uncontrolled leukemia
IV-209. Patients with all of the following conditions have increased risk of developing mucormycosis EXCEPT:
A. Deferoxamine therapy
B. Factitious hypoglycemia
C. Glucocorticoid therapy
D. Metabolic acidosis
E. Neutropenia
| FIGURE IV-210 (see Color Atas) A. Hemodialysis B. Insulin C. Liposomal amphotericin B |
IV-210. A 36-year-old woman with a history of diabetes mellitus, hypertension, and chronic renal insufficiency reports comes to the emergency department complaining of double vision for 1 day. She is on chronic hemodialysis and missed her last appointment. She also notes 12 hours of facial swelling and difficulty speaking. Her vital signs are notable for a temperature of 39.0°C and blood pressure 155/95 mmHg. Her facial examination is shown in Figure IV-210. Laboratory examination reveals a white blood cell count of 15,000/μL, serum glucose of 205 mg/dL, serum creatinine of 6.3 mg/dL, and hemoglobin A1c of 9.7%. Arterial blood gas on room air is pH of 7.24, PCO2 of 20 mmHg, and PO2 of 100 mmHg. Needle biopsy of a retro-orbital mass reveals wide, thick–walled, ribbon-shaped nonseptate hyphal organisms that branch at 90 degrees with tissue and vascular invasion on PAS stain. All of the following are components of the initial therapy EXCEPT:

D. Surgical debridement
E. Voriconazole
IV-211. Which of the following is the most common form of infection in patients with mucormycosis?
A. Cutaneous
B. Gastrointestinal
C. Hematogenous dissemination
D. Pulmonary
E. Rhinocerebral
IV-212. A 21-year-old college student seeks your opinion because of a lesion on his head. He has no significant medical history and reports a solitary lesion on the crown of his head for more than month that has been growing slowly. He has had no fever and reports that although the area is itchy, he feels well. On examination, you note a 3-cm round area of alopecia without redness, pain, or inflammation. It is well demarcated with central clearing, scaling, and broken hair shafts at the edges. There is no redness or pain. Which of the following should you recommend?
A. Caspofungin
B. Clindamycin
C. Doxycycline
D. Minoxidil
E. Terbinafine
IV-213. A 68-year-old woman seeks evaluation for an ulcerative lesion on her right hand. She reports that the area on the back of her right hand was initially red and not painful. There appeared to be a puncture wound in the center of the area, and she thought she had a simple scratch acquired while gardening. Over the next several days, the lesion became verrucous and ulcerated. Now the patient has noticed several nodular areas along the arm, one of which ulcerated and began draining a serous fluid today. She is also noted to have an enlarged and tender epitrochlear lymph node on the right arm. A biopsy of the edge of the lesion shows ovoid and cigar-shaped yeasts. Sporotrichosis is diagnosed. What is the most appropriate therapy for this patient?
A. Amphotericin B intravenously
B. Caspofungin intravenously
C. Clotrimazole topically
D. Itraconazole orally
E. Selenium sulfide topically
IV-214. A 35-year-old woman with long-standing rheumatoid arthritis has been treated with infliximab for the past 6 months with improvement of her joint disease. She has a history of positive PPD and takes INH prophylaxis. For the past week, she reports worsening dyspnea on exertion with low-grade fevers and a nonproductive cough. On examination, her vital signs are notable for normal blood pressure, temperature of 38.0°C, heart rate of 105 beats/min, respiratory rate of 22 breaths/min, and SaO2 of 91%
on room air. Her lungs are clear. Within one flight of steps, she becomes dyspneic, and her SaO 2 falls
to 80%. A chest CT scan is shown in Figure IV-214. Which of the following is the most likely
diagnosis?
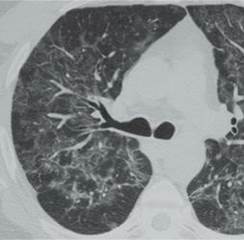
FIGURE IV-214
A. Aspergillus fumigatus pneumonia
B. Nocardia asteroides pneumonia
C. Pneumocystis jiroveci pneumonia
D. Rheumatoid nodules
E. Staphylococcal bacteremia and septic pulmonary emboli
IV-215. Which of the following patients should receive prophylaxis against Pneumocystis jiroveci pneumonia?
A. A 19-year-old woman with acute myelogenous leukemia initiating induction chemotherapy
B. A 24-year-old man with HIV initiated on HAART therapy 9 months ago when his CD4 count
was 100/μL and now has a CD4 count of 500/μL for the past 4 months
C. A 36-year-old man with newly diagnosed HIV and a CD4 count of 300/μL
D. A 42-year-old woman with rheumatoid arthritis who recovered from an episode of
Pneumocystis pneumonia while taking infliximab who is now initiating therapy with abatacept
E. A 56-year-old man with COPD receiving prednisone for an acute exacerbation
IV-216. A 45-year-old woman with known HIV infection and medical nonadherence to therapy is admitted to the hospital with 2 to 3 weeks of increasing dyspnea on exertion and malaise. A chest radiograph shows bilateral alveolar infiltrates, and induced sputum is positive for Pneumocystis jiroveci. Which of the following clinical conditions is an indication for administration of adjunct glucocorticoids?
A. Acute respiratory distress syndrome
B. CD4+ lymphocyte count <100/μL
C. No clinical improvement 5 days into therapy
D. Pneumothorax
E. Room air PaO2 <70 mmHg
IV-217. All of the following statements regarding the drug mefloquine are true EXCEPT:
A. Dose adjustment is necessary in patients with renal insufficiency.
B. It is only available in oral form.
C. It is the preferred drug for prophylaxis of chloroquine-resistant malaria.
D. It should not be administered concurrently with halofantrine.
E. Psychiatric side effects limit it use in certain patients.
IV-218. A 45-year-old migrant worker originally from Mexico is evaluated for right upper quadrant pain, fever, and hepatic tenderness. He reports no diarrhea or bloody stool. He is found to have a large hepatic abscess on CT scan of the abdomen. Of note, he has been in the United States for approximately 10 years and was well until approximately 10 days ago. Which of the following tests can be used to confirm the diagnosis?
A. Examination of stool for trophozoites
B. Liver biopsy
C. PCR of stool for Campylobacter spp.
D. Response to empiric trial of iodoquinol
E. Serologic test for antibody to E. histolytica
IV-219. A 23-year-old woman is seen in the emergency department for fever and altered mental status. She is from Tanzania and arrived in the United States earlier that day. She reported 3 days of episodic fever before leaving home. Over the course of the day, her family describes deteriorating mental status.
Now she is confused and lethargic. Her physical examination is notable for a temperature of 40°C, heart rate of 145 beats/min, and systemic blood pressure of 105/62 mmHg. She has a clearly gravid uterus, approximately 24 weeks of gestational age, and a neurologic examination shows confusion but no focal findings. A thick and thin smear are shown in Figure IV-219. Treatment with IV quinidine is started immediately. Which of the followings are potential complications of this therapy?
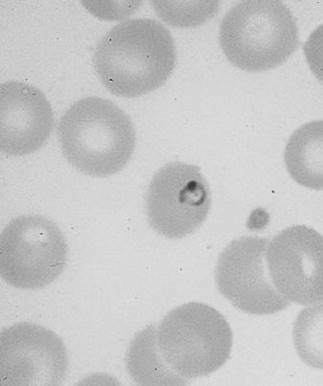
FIGURE IV-219 (see Color Atas)
A. Hyperthyroidism
B. Hypoglycemia
C. Nightmares
D. Retinopathy
E. Seizures
IV-220. A 20-year-old man is seen in the university walk-in health clinic for evaluation of recurrent fever. He reports fever greater than 101°F lasting less than a day occurring approximately weekly for the past 3 weeks. He feels otherwise relatively poorly with diffuse myalgias and headache that are much worse during the febrile episodes. Of note, he returned recently from a mission trip to Central America and reports not taking malaria prophylaxis. Examination of the peripheral smear confirms the diagnosis of Plasmodium vivax. If present, which of the following findings indicates that the patient has severe malaria and is not a candidate for outpatient therapy?
A. Fever >40°C
B. One seizure last week
C. Parasitemia of >5% affected erythrocytes on peripheral smear
D. Serum bilirubin level of >2 mg/dL
E. The presence of headache
IV-221. A 51-year-old woman is diagnosed with Plasmodium falciparum malaria after returning from a safari in Tanzania. Her parasitemia is 6%, hematocrit is 21%, bilirubin is 7.8 mg/dL, and creatinine is 2.7 mg/dL. She is still making 60 mL/hr of urine. She rapidly becomes obtunded. Intensive care is initiated with frequent creatinine checks, close monitoring for hypoglycemia, infusion of phenobarbital for seizure prevention, mechanical ventilation for airway protection, and exchange transfusion to address her high parasitemia. Which of the following regimens is recommended as first-line treatment for her malarial infection?
A. Chloroquine
B. Intravenous artesunate
C. Intravenous quinine
D. Intravenous quinidine
E. Mefloquine
IV-222. A 28-year-old woman presents with fevers, headache, diaphoresis, and abdominal pain 2 days after returning from an aid mission to the coast of Papua New Guinea. Several of her fellow aid workers developed malaria while abroad, and she stopped her doxycycline prophylaxis because of a photosensitivity reaction 5 days earlier. You send blood cultures, routine labs, and a thick and thin smear to evaluate the source of her fevers. Which of the following statements is accurate in reference to diagnosis of malaria?
A. A thick smear is performed to increase sensitivity compared with a thin smear but can only be
performed in centers with experienced laboratory personnel and has a longer processing time.
B. Careful analysis of the thin blood film allows for prognostication based on estimation of
parasitemia and morphology of the erythrocytes.
C. In the absence of rapid diagnostic information, empirical treatment for malaria should be
strongly considered.
D. Morphology on blood smear is the current criterion used to differentiate the four species of
Plasmodium that infect humans.
E. All of the above are true.
IV-223. A 19-year-old college student is employed during the summer months on Nantucket Island in Massachusetts. She is evaluated in the local emergency department with 5 days of fever, malaise, and generalized weakness. Although she does recall a tick bite approximately 6 weeks ago, she denies rash around that time or presently. Physical examination is unremarkable with the exception of a temperature of 39.3°C. Which of the following statements is true regarding her most likely illness?
A. B. duncani is the most likely organism to be found in her peripheral blood smear.
B. First-line therapy for severe disease in this patient is immediate complete RBC exchange
transfusion in addition to clindamycin and quinine.
C. If babesiosis is not demonstrated on thick or thin preparations of peripheral blood, PCR
amplification of babesial 18S rRNA is recommended.
D. The ring form of B. microti seen in red blood cells on microscopy is indistinguishable from
Plasmodium falciparum.
E. Without a current or historical rash, she is unlikely to have babesiosis.
IV-224. A 35-year-old man from India is seen for evaluation of several weeks of fever that has decreased in intensity, but he now has developed abdominal swelling. He has no significant past medical history. Physical examination shows palpable splenomegaly and hepatomegaly and diffuse lymphadenopathy. Diffuse hyperpigmentation is present in his skin. Visceral leishmaniasis is suspected. Which of the following diagnostic techniques is most commonly used?
A. Culture of peripheral blood for Leishmania spp.
B. PCR for L. infantum nucleic acid in peripheral blood
C. Rapid immunochromatographic test for recombinant antigen rK39 from L. infantum
D. Smear of stool for amastigotes
E. Splenic aspiration to demonstrate amastigotes
IV-225. All of the following statements regarding infection with Trypanosoma cruzi are true EXCEPT:
A. It is found only in the Americas.
B. It is the causative agent of Chagas disease.
C. It is transmitted to humans by the bite of deer flies.
D. It may be transmitted to humans by blood transfusion.
E. It may cause acute and chronic disease.
IV-226. A 36-year-old man is admitted to the hospital with 3 months of worsening dyspnea on exertion and orthopnea. Over the past 2 weeks, he has been sleeping upright. He denies any chest pain with exertion or syncope. There is no history of hypertension, hyperlipidemia, or diabetes. He is a lifelong nonsmoker and since arriving to the United States from rural Mexico 16 years ago works as an electrician. His physical examination is notable for being afebrile with a heart rate 105 beats/min, blood pressure of 100/80 mmHg, respiratory rate of 22 breaths/min, and oxygen saturation of 88% on room air. He has notable jugular venous distension upright with no Kussmaul sign, 3+ pitting edema to the knees, and bilateral crackles two-thirds up the lung fields. Cardiac examination shows a laterally displaced PMI, a 2/6 systolic murmur at the apex and axilla, an S3, and no friction rub or pericardial knock. Which of the following is likely to reveal the most likely diagnosis?
A. Coronary angiography
B. Right heart catheterization
C. Serum PCR for T. cruzi DNA
D. Serum T. cruzi IgG antibodies
E. Serum troponin
IV-227. A 36-year-old medical missionary recently returned from a 2-week trip to rural Honduras. During the trip, she lived in the jungle, where she received multiple bug bites and developed open sores. One week after her return, she comes to the clinic reporting 2 days of malaise, fever to 38.5°C, and anorexia. There is an indurated swollen area of erythema on her calf and femoral adenopathy. Because of her exposure history, you obtain a thin and thick blood smear that demonstrates organisms consistent with T. cruzi. Which of the following is the best next intervention?
A. Immediate therapy with benznidazole
B. Immediate therapy with primaquine
C. Immediate therapy with voriconazole
D. Observation only
E. Serologic confirmation with specific T. cruzi IgG testing
IV-228. A 44-year-old man who recently returned from a safari trip to Uganda seeks attention for a painful lesion on the leg and new fevers. He was on a safari tour, where he stayed in the animal park that was populated extensively with antelope, lions, giraffes, and hippos. They often toured savannah and jungle settings. He returned within the past week and noticed a painful lesion on his neck at the site of some bug bites. He reports fever over 38°C, and you find palpable cervical lymphadenopathy. Review of systems is notable for malaise and anorexia for 2 days. A thick and thin smear of the blood reveals protozoa consistent with trypanosomes. All of the following are true about his disease EXCEPT:
A. Humans are the primary reservoir.
B. If untreated, death is likely.
C. It was transmitted by the bite of a tsetse fly.
D. Lumbar puncture should be performed.
E. Suramin is effective treatment.
IV-229. A 36-year-old man with HIV/AIDS is brought to the hospital after a grand mal seizure at home. He has a history of ongoing IV drug use and is not taking HAART. His last CD4 T-cell count was below 50/μL more than 1 month ago. Further medical history is unavailable. Vital signs are normal. On examination, he is barely arousable and disoriented. He is cachectic. There is no nuchal rigidity or focal motor deficits. Serum creatinine is normal. An urgent head MRI with gadolinium is performed, and the results of the T1-gated images are shown in Figure IV-229. Which of the following will be the most effective therapy?
A. Caspofungin
B. INH, rifampin, PZA, and ethambutol
C. Pyrimethamine plus sulfadiazine
D. Streptokinase
E. Voriconazole
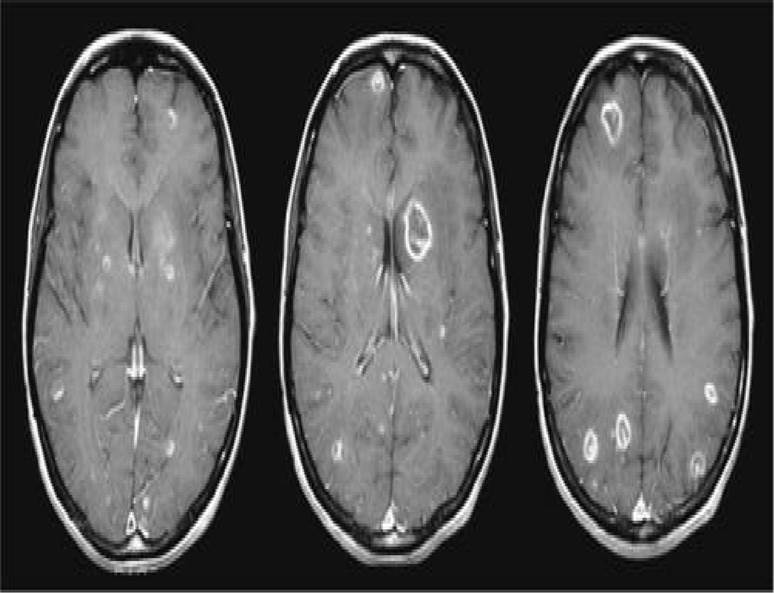
FIGURE IV-229
IV-230. Which of the following intestinal protozoal infections can be diagnosed with stool ova and parasite examination?
A. Cryptosporidium spp.
B. Cyclospora spp.
C. Giardia spp.
D. Isospora spp.
E. Microsporidia spp.
F. All of the above
IV-231. A 17-year-old woman presents to the clinic complaining of vaginal itchiness and malodorous discharge. She is sexually active with multiple partners, and she is interested in getting tested for sexually transmitted diseases. A wet-mount microscopic examination is performed, and trichomonal parasites are identified. Which of the following statements regarding trichomoniasis is true?
A. A majority of women are asymptomatic.
B. No treatment is necessary because the disease is self-limited.
C. The patient’s sexual partner need not be treated.
D. Trichomoniasis can only be spread sexually.
E. Trichomoniasis is 100% sensitive to metronidazole
IV-232. A 19-year-old college student presents to the emergency department with crampy abdominal pain and watery diarrhea that has worsened over 3 days. He recently returned from a volunteer trip to Mexico. He has no past medical history and felt well throughout the trip. Stool examination shows small cysts containing four nuclei, and stool antigen immunoassay is positive for Giardia spp. Which of the following is a recommend treatment regimen for this patient?
A. Albendazole
B. Clindamycin
C. Giardiasis is self-limited and requires no antibiotic therapy
D. Paromomycin
E. Tinidazole
IV-233. A 28-year-old woman is brought to the hospital because of abdominal pain, weight loss, and dehydration. She has been diagnosed with HIV/AIDS for the past 2 years with a history of oral candidiasis and pneumocystis pneumonia. She reports voluminous watery diarrhea over the past 2 weeks. Because of medical nonadherance, she has not taken any antiretroviral therapy. Routine stool ova and parasite examination is normal, but stool antigen testing reveals Cryptosporidium spp. Which of the following is the recommended therapy?
A. Metronidazole
B. Nitazoxanide
C. No therapy recommended because the diarrhea is self-limited.
D. No effective specific therapy is available.
E. Tinidazole
IV-234. Which of the following has resulted in a significant decrease in the incidence of trichinellosis in the United States?
A. Adequate therapy that allows for eradication of infection in index cases before person-to-person
spread can occur
B. Earlier diagnosis because of a new culture assay
C. Federal laws limiting the import of foreign cattle
D. Laws prohibiting the feeding of uncooked garbage to pigs
E. Requirements for handwashing by commercial kitchen staff who handle raw meat
IV-235. A patient comes into the clinic and describes progressive muscle weakness over several weeks. He has also experienced nausea, vomiting, and diarrhea. One month ago, he had been completely healthy and describes a bear hunting trip in Alaska, where they ate some of the game they killed. Soon after he returned, his gastrointestinal symptoms began followed by muscle weakness in his jaw and neck that has now spread to his arms and lower back. Examination confirms decreased muscle strength
in the upper extremities and neck. He also has slowed extraocular movements. Laboratory examination shows panic values for elevated eosinophils and serum creatine phosphokinase. Which of the following organisms is most likely the cause of his symptoms?
A. Campylobacter spp.
B. Cytomegalovirus
C. Giardia spp.
D. Taenia solium
E. Trichinella spp.
IV-236. A 3-year-old boy is brought by his parents to the clinic. They state that he has experienced fevers, anorexia, weight loss, and most recently has started wheezing at night. He had been completely healthy until these symptoms started 2 months ago. The family had travelled through Europe several months earlier and reported no unusual exposures or exotic foods. They have a puppy at home. On examination, the child is ill-appearing and is noted to have hepatosplenomegaly. Laboratory results show a panic value of 82% eosinophils. Total white blood cells are elevated. A complete blood count is repeated to rule out a laboratory error, and eosinophils are 78%. Which of the following is the most likely organism or process?
A. Cysticercus spp.
B. Giardiasis
C. Staphylococcus lugdunensis
D. Toxocariasis
E. Trichinellosis
IV-237. The patient described above continues to decline over the next 2 to 3 days, developing worsening respiratory status, orthopnea, and cough. On physical examination, his heart rate is 120 beats/min, blood pressure is 95/80 mmHg, respiratory rate is 24 breaths/min, and oxygen saturation is 88% on room air. His neck veins are elevated, there is an apical S3, and his lungs have bilateral crackles halfway up the lung fields. An echocardiogram shows an ejection fraction of 25%. Which of the following therapies should be initiated?
A. Albendazole
B. Methylprednisolone
C. Metronidazole
D. Praziquantel
E. Vancomycin
IV-238. A 28-year-old man is brought to the emergency department by his wife for altered mental status, fevers, vomiting, and headache. He developed a bilateral headache began about 1 day ago that has progressively worsened. He and his wife returned from a trip to Thailand and Vietnam, where they spent a lot of time in rural settings eating local mollusks, seafood, and vegetables. His physical examination is notable for fever, nuchal rigidity, confusion, and lethargy. Lumbar puncture reveals elevated opening pressure; elevated protein; normal glucose; and white blood cell count of 200/μL with 50% eosinophils, 25% neutrophils, and 25% lymphocytes. Which of the following is the most likely etiology of his meningitis?
Date: 2016-04-22; view: 1751
| <== previous page | | | next page ==> |
| ÀÌìÉÀæDVT, Jeep venous [Û)ÛêÐÅ, pulmonary embolism. 5 page | | | ÀÌìÉÀæDVT, Jeep venous [Û)ÛêÐÅ, pulmonary embolism. 7 page |