
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
ÀÌìÉÀæDVT, Jeep venous [Û)ÛêÐÅ, pulmonary embolism. 1 page
TTT-112. The answer is C.(Chap. 118) In recent years, a variety of new anticoagulant and antiplatelet drugs have been developed for clinical use. Platelets play an important role in arterial thrombosis, particularly in coronary artery and cerebrovascular disease. Aspirin is the most widely used antiplatelet drug worldwide. Aspirin exerts its effects through inhibition of cyclooxygenase-1. Other commonly used oral antiplatelet agents are clopidogrel and dipyridamole. Clopidogrel is in a class of agents called thienopyridines along with ticlopidine. Thienopyridines act to block a specific adenosine diphosphate receptor (P2Y12) and inhibit platelet aggregation. Dipyridamole inhibits phosphodiesterase
to decrease the breakdown of cyclic adenosine monophosphate (cAMP) to decrease platelet aggregation. Intravenous antiplatelet agents have also become increasingly important in the treatment of acute coronary syndromes. All of the intravenous agents act to inhibit platelet aggregation by blocking the glycoprotein (GP) Ilb/IIIa receptor. The three agents in clinical use as GP Ilb/IIIa inhibitors are abciximab, eptifibatide, and tirofiban.
Anticoagulant agents are primarily used for the prevention and treatment of venous thrombosis. Many anticoagulants are available and act by a variety of mechanisms. Heparin has been used for many years but requires frequent monitoring to be used safely. More recently, low-molecular-weight heparins (LMWHs) have been introduced. These agents are given subcutaneously and generally preferred in many instances over heparin given a more predictable anticoagulant effect. Both heparin and the LMWHs are indirect thrombin inhibitors that act primarily through activation of antithrombin. When activated, antithrombin inhibits clotting enzymes, especially thrombin and factor Xa. Fondaparinux is a newer anticoagulant that inhibits only factor Xa, although it is a synthetic analogue of the
pentasaccharide sequence in heparin that binds antithrombin. However, it is too short to bridge antithrombin to thrombin. The direct thrombin inhibitors bind directly to thrombin (rather than antithrombin) to exert their activity. The direct thrombin inhibitors include lepirudin, argatroban, and bivalirudin. The most commonly used oral anticoagulant is warfarin, which inhibits the production of vitamin K-dependent clotting factors. Given the need for frequent monitoring and extensive drug interactions, developing other oral anticoagulants that are safe and effective has been desired for many years. No oral drug has yet been introduced into the market. However, several are in the final stages of development. These include two factor Xa inhibitors (rivaroxaban and apixaban) and one factor Ha inhibitor (dabigatran etexilate).
TTT-113. The answer is B.(Chap. 118) After implantation of a bare metal coronary artery stent, aspirin and clopidogrel are recommended for at least 4 weeks to decrease the risk of instent restenosis. This patient, however, developed the complication despite adherence to her therapy. This generally suggests resistance to clopidogrel with a decreased ability of clopidogrel to inhibit platelet aggregation. There is a known genetic component to clopidogrel resistance related to specific genetic polymorphisms of the CYP isoenzymes. Up to 25% of whites, 30% of African Americans, and 50% of Asians may carry an allele that renders them resistant to clopidogrel. These polymorphisms are less important in the activation of prasugrel. Thus, in individuals who have evidence of clopidogrel resistance, switching to prasugrel should be considered.
Aspirin resistance is a more controversial subject. It is defined simply in clinical terms as failure of aspirin to prevent ischemic vascular events. Biochemically, aspirin resistance can be defined by failure of usual doses of the drug to produce inhibitory effects on platelet function. However, resistance to aspirin is not reversed by higher doses of aspirin or adding another antiplatelet agent. Because the primary mechanism of arterial thrombosis is platelet aggregation, the anticoagulant agents warfarin and low-molecular-weight heparin are not indicated.
TTT-114. The answer is B.(Chap. 118) Low-molecular-weight heparins (LMWHs) have largely replaced heparin for most indications if a patient does not have any contraindications to therapy. LMWHs have better bioavailability and longer half-lives after subcutaneous injection. Thus, they can be given at routine intervals for both prophylaxis and treatment. In addition, dosing of LMWHs is simplified because these drugs have a dose-independent clearance, and predictable anticoagulant effects means that monitoring of anticoagulant effect is not required in most patients. Finally, LMWHs have a lower risk of heparin-induced thrombocytopenia, which is important in both short- and long-term administration.
SECTION IV Infectious Diseases
QUESTION
DIRECTIONS: Choose the one best response to each question.
IV-1. Deficits in the complement membrane attack complex (C5-8) are associated with infections of what variety?
A. Catalase-positive bacteria
B. Neisseria meningitis
C. Pseudomonas aeruginosa
D. Salmonella spp.
E. Streptococcus pneumoniae
IV-2. A 48-year-old man is admitted to the intensive care unit for treatment of septic shock for an uncertain cause. He was well until 1 day before admission. His family reports that he developed myalgias and fevers at that time. He had no other specific complaints but reportedly had decreased oral intake and generalized malaise. He was brought to the hospital by ambulance this morning when he was lethargic and unresponsive at home. Upon arrival of emergency medical services, his initial blood pressure was 60/40 mmHg with a heart rate of 142 beats/min. He was tachypneic with a respiratory rate of 32 breaths/min with an oxygen saturation of 75% on room air, and his initial temperature was 104.9°F (40.5°C). He was intubated and placed on mechanical ventilation. The patient received 1 L of normal saline before arrival in the emergency department but continues to have hypotension (blood pressure, 75/40 mmHg). Ongoing volume resuscitation is ordered, and the patient is initiated on norepinephrine to maintain adequate blood pressure. The patient has a history of hypertension and hyperlipidemia. He takes amlodipine 10 mg daily and atorvastatin 20 mg daily. His only other history is an automobile accident at age 20 years, requiring exploratory laparotomy and splenectomy. Blood, sputum, and urine cultures are obtained. What are the most appropriate empiric antibiotics for the treatment of this patient?
A. Ceftriaxone and vancomycin
B. Ceftriaxone, ampicillin, and vancomycin
C. Ceftriaxone, vancomycin, and amphotericin B
D. Clindamycin, gentamicin, and vancomycin
E. Clindamycin and quinine
IV-3. A 32-year-old woman is admitted to the hospital complaining of right thigh pain. She is treated empirically with oxacillin intravenously for a cellulitis. The admitting physician notes that the degree of pain appears to be disproportionate to the amount of overlying cellulitis. Over the course of the next 24 hours, the patient develops profound septic shock complicated by hypotension, acute renal failure, and
evidence of disseminated intravascular coagulation. A CT scan of her right leg demonstrates a collection of fluid with gas in the deep fascia of her right leg. Emergent surgical evacuation is planned. What changes to the patient’s antibiotic therapy would be recommended?
A. Continue oxacillin and add clindamycin.
B. Continue oxacillin and add clindamycin and gentamicin.
C. Discontinue oxacillin and add clindamycin, vancomycin, and gentamicin.
D. Discontinue oxacillin and add piperacillin/tazobactam and vancomycin.
E. Discontinue oxacillin and add vancomycin and gentamicin.
IV-4. Which type of bite represents a potential medical emergency in a febrile asplenic patient?
A. Cat bite
B. Dog bite
C. Fish bite
D. Human bite
IV-5. One goal of immunization programs is to eliminate a specific disease. In 2010, indigenous transmission of which of the following diseases had been eliminated in the United States?
A. Diphtheria
B. Mumps
C. Pertussis
D. Varicella
E. None of the above
IV-6. A 63-year-old man has chronic obstructive pulmonary disease and presents to your office for routine follow-up. He has no complaints currently and feels well. He is being managed with tiotropium 18 μg once daily with albuterol metered-dose inhaler as needed. His most recent forced expiratory volume in 1 second (FEV1) was 55% predicted, and he is not on oxygen. He has received one dose of
pneumococcal vaccine 5 years previously. He is asking if he should receive another dose of pneumococcal vaccine. According to the guidelines of the Centers for Disease Control and Prevention, what is your recommendation?
A. He does not require further vaccination unless his FEV1 drops below 50% predicted.
B. He does not require further vaccination until he reaches age 65 years.
C. He should be revaccinated today.
D. He should be revaccinated 10 years after his initial vaccine.
E. No further vaccination is recommended because a single dose is all that is required.
IV-7. In which of the following patients is it appropriate to administer the vaccination against herpes zoster?
A. A 35-year-old woman who has never had varicellazoster infection who is 12 weeks pregnant
with her first child
B. A 54-year-old man who has never had varicellazoster infection and is otherwise healthy
C. A 62-year-old man with HIV on antiretroviral therapy with a CD4+ lymphocyte count of 450/μL
D. A 64-year-old woman with dermatomyositis-associated interstitial lung disease treated with
prednisone 20 mg daily and azathioprine 150 mg daily
E. A 66-year-old woman who was recently diagnosed with non-Hodgkin lymphoma
IV-8. A 39-year-old woman received a liver transplant 2 years ago and is maintained on prednisone, 5 mg, and cyclosporine, 8 mg/kg per day. She has had two episodes of rejection since transplant, as well an episode of cytomegalo-virus syndrome and Nocardia pneumonia. She intends on taking a 2-week gorilla-watching trip to Rwanda and seeks your advice regarding her health while abroad. Which of the following potential interventions is strictly contraindicated?
A. Malaria prophylaxis
B. Meningococcal vaccine
C. Rabies vaccine
D. Typhoid purified polysaccharide vaccine
E. Yellow fever vaccine
IV-9. A 19-year-old woman comes to your office after being bitten by a bat on the ear while camping in a primitive shelter. She is unable to produce a vaccination record. On physical examination, she is afebrile and appears well. There are two small puncture marks on the pinna of her left ear. What is an appropriate vaccination strategy in this context?
A. Intravenous ribavirin
B. No vaccination
C. Rabies immunoglobulins
D. Rabies inactivated virus vaccine
E. Rabies inactivated virus vaccine plus immunoglobulins
IV-10. Which of the following immunizations is required for entry into many countries in sub-Saharan Africa?
A. Hepatitis A
B. Cholera
C. Meningococcus
D. Typhoid fever
E. Yellow fever
IV-11. A 48-year-old woman is traveling to Haiti with a humanitarian aid group. What is the recommended prophylaxis against malaria for this patient?
A. Atovaquone–proguanil
B. Chloroquine
C. Doxycycline
D. Mefloquine
E. Any of the above can be used
IV-12. A 46-year-old man wishes to travel to Kenya for a 2-week vacation. He is HIV positive and is taking antiretroviral therapy. His last CD4+ count was 625/μL and viral load was undetectable. His nadir CD4+ count was 250/μL. He has never had an AIDS-defining illness. In addition to HIV, he has a history of hypertension and is known to have proteinuria caused by to HIV-associated nephropathy. What is your recommendation to this patient regarding his travel plans?
A. He should not receive the live measles vaccine before travel.
B. He should receive the yellow fever vaccine before travel.
C. He will be required to show proof of HIV testing upon entry into the country.
D. His likelihood of response to the influenza vaccine would be less than 50%.
E. With a CD4+ count greater than 500/μL, he is at no greater risk during travel than persons
without HIV.
IV-13. Which of the following is the most common cause of native valve infective endocarditis in the community?
A. Coagulase-negative staphylococci
B. Coagulase-positive staphylococci
C. Enterococci
D. Fastidious gram-negative coccobacilli
E. Non-enterococcal streptococci
IV-14. All of the following are minor criteria in the Duke criteria for the clinical diagnosis of infective endocarditis EXCEPT:
A. Immunologic phenomena (glomerulonephritis, Osler nodes, Roth spots)
B. New valvular regurgitation on transthoracic echo-cardiogram
C. Predisposing condition (heart condition, intravenous drug use)
D. Temperature >380°C
E. Vascular phenomena (arterial emboli, septic pulmonary emboli, Janeway lesions, and so on)
IV-15. Which of the following patients should receive antibiotic prophylaxis to prevent infective endocarditis?
A. A 23-year-old woman with known mitral valve prolapse undergoing a gingival surgery
B. A 24-year-old woman who had an atrial septal defect completely corrected 22 years ago who is
undergoing elective cystoscopy for painless hematuria
C. A 30-year-old man with a history of intravenous drug use and prior endocarditis undergoing
operative drainage of a prostatic abscess
D. A 45-year-old man who received a prosthetic mitral valve 5 years ago undergoing routine dental
cleaning
E. A 63-year-old woman who received a prosthetic aortic valve 2 years ago undergoing screening
colonoscopy
IV-16. A 38-year-old homeless man presents to the emergency department with a transient ischemic attack characterized by a facial droop and left arm weakness lasting 20 minutes and left upper quadrant
pain. He reports intermittent subjective fevers, diaphoresis, and chills for the past 2 weeks. He has had no recent travel or contact with animals. He has taken no recent antibiotics. Physical examination reveals a slightly distressed man with disheveled appearance. His temperature is 38.2°C, heart rate is 90 beats/min, and blood pressure is 127/74 mmHg. He has poor dentition. Cardiac examination reveals an early diastolic murmur over the left third intercostal space. His spleen is tender and 2 cm descended below the costal margin. He has tender painful red nodules on the tips of the third finger of his right hand and on the fourth finger of his left hand that are new. He has nits evident on his clothes consistent with body louse infection. His white blood cell count is 14,500/μL with 5% band forms and 93% polymorphonuclear cells. Blood cultures are drawn followed by empirical vancomycin therapy. These cultures remain negative for growth 5 days later. He remains febrile but hemodynamically stable but does develop a new lesion on his toe similar to those on his fingers on hospital day 3. A transthoracic echocardiogram reveals a 1-cm mobile vegetation on the cusp of his aortic valve and moderate aortic regurgitation. A CT scan of the abdomen shows an enlarged spleen with wedge-shaped splenic and renal infarctions. What test should be sent to confirm the most likely diagnosis?
A. Bartonella serology
B. Epstein-Barr virus (EBV) heterophile antibody
C. HIV polymerase chain reaction (PCR)
D. Peripheral blood smear
E. Q fever serology
IV-17. In a patient with bacterial endocarditis, which of the following echocardiographic lesions is most likely to lead to embolization?
A. 5-mm mitral valve vegetation
B. 5-mm tricuspid valve vegetation
C. 11-mm aortic valve vegetation
D. 11-mm mitral valve vegetation
E. 11-mm tricuspid valve vegetation
IV-18. A patient is admitted with fevers, malaise, and diffuse joint pains. His initial blood cultures reveal methicillin-resistant Staphylococcus aureus (MRSA) in all culture bottles. He has no arthritis on examination, and his renal function is normal. Echocardiogram shows a 5-mm vegetation on the aortic valve. He is initiated on IV vancomycin at 15 mg/kg every 12 hours. Four days later, the patient remains febrile, and cultures remain positive for MRSA. In addition to a search for embolic foci of infection, which of the following changes would you make to his treatment regimen?
A. No change.
B. Add gentamicin.
C. Add rifampin.
D. Check the vancomycin serum peak and trough levels and consider tid dosing.
E. Discontinue vancomycin, start daptomycin.
IV-19. All of the following organisms may cause bullae as a manifestation of their infection except: A. Clostridium perfringens
B. Sporothrix schenckii
C. Staphylococcus aureus
D. Streptococcus pyogenes
E. Vibrio vulnificus
IV-20. A 24-year-old man with no past medical history is brought to the emergency department complaining of left-sided chest pain for 2 days. He reports the skin over his left chest is tender and swollen. He has no history of HIV risk behavior and works as a landscaper. His physical examination is notable for a heart rate of 110 beats/min, blood pressure of 108/62 mmHg, and temperature of 101.8°F. He has pain and swelling of the left chest. His electrocardiogram is normal. A noncontrast CT scan of the chest (Figure IV-20) is obtained. Which of the following organisms is most likely causing his illness?
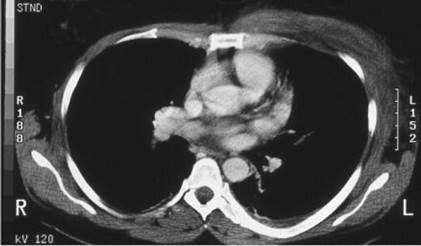
FIGURE IV-20
A. Coxsackie virus A16
B. Mycobacterium tuberculosis
C. Rickettsia akari
D. Streptococcus pyogenes
E. Varicella-zoster virus
IV-21. All of the following statements regarding the etiology and epidemiology of osteomyelitis are true EXCEPT:
A. After a foot puncture, 30% to 40% of patients with diabetes develop osteomyelitis.
B. In patients with prosthetic joints, Staphylococcus aureus bacteremia will cause osteomyelitis in
25% to 30% of cases.
C. Mycobacterium tuberculosis is an uncommon cause of osteomyelitis.
D. The foremost bacterial cause of osteomyelitis is Staphylococcus aureus.
E. The morbidity and economic consequences of MRSA osteomyelitis are greater than for MSSA
osteomyelitis.
IV-22. A 79-year-old man has had a diabetic foot ulcer overlying his third metatarsal head for 3 months
but has not been compliant with his physician’s request to offload the affected foot. He presents with dull, throbbing foot pain and subjective fevers. Examination reveals a putrid-smelling wound notable also for a pus-filled 2.5-cm-wide ulcer. A metal probe is used to probe the wound, and it detects bone as well as a 3-cm deep cavity. Gram stain of the pus shows gram-positive cocci in chains, gram-positive rods, gram-negative diplococci, enteric-appearing gram-negative rods, tiny pleomorphic gram-negative rods, and a predominance of neutrophils. Which of the following empirical antibiotic regimens is recommended while blood and drainage cultures are processed?
A. Ampicillin–sulbactam, 1.5 g IV q4h
B. Clindamycin, 600 mg PO tid
C. Linezolid, 600 mg IV bid
D. Metronidazole, 500 mg PO qid
E. Vancomycin, 1 g IV bid
IV-23. A 45-year-old man with a history of alcoholism and presumed cirrhosis is brought to the emergency department by his friend complaining of 2 to 3 days of increasing lethargy and confusion. He has not consumed alcohol in the past 2 years. He currently takes no medications and works at home as a video game designer. He has no risk factors for HIV. He was referred by his primary care physician for a liver transplant evaluation and is scheduled to begin his evaluation next month. His vital signs included blood pressure of 90/60 mmHg, heart rate of 105 beats/min, temperature of 38.5°C, and respiratory rate of 10 breaths/min with O2 saturation of 97% on room air. He is somnolent but is able to
answer questions accurately. His skin is notable for many spider telangiectasias and palmar erythema. He has a distended diffusely tender abdomen with a positive fluid wave. Paracentesis reveals slightly cloudy fluid with WBC 1000/μL and 40% neutrophils. His blood pressure increases to 100/65 mmHg, and his heart rate decreases to 95 beats/min after 1 L of intravenous fluids. Which of the following statements regarding his condition and treatment is true?
A. Fever is present in more than 50% of cases.
B. Initial empiric therapy should include metronidazole or clindamycin for anaerobes.
C. The diagnosis of primary (spontaneous) bacterial peritonitis is not confirmed because the
percentage of neutrophils in the peritoneal fluid is less than 50%.
D. The mostly causative organism for his condition is enterococcus.
E. The yield of peritoneal fluid cultures for diagnosis is greater than 90%.
IV-24. A 48-year-old woman with a history of end-stage renal disease caused by diabetic renal disease is admitted to the hospital with 1 day of abdominal pain and fever. She has been on continuous ambulatory peritoneal dialysis (CAPD) for the past 6 months. She reports that for the past day she has had poor return of dialysate and is feeling bloated. She has had complications from her diabetes, including retinopathy and peripheral neuropathy. She is uncomfortable but not toxic. Her vital signs include a temperature of 38.8°C, blood pressure of 130/65 mmHg, heart rate of 105 beats/min, and respiratory rate of 15 breaths/min with room air O2 saturation of 98%. Her abdomen is slightly distended and
diffusely tender with rebound tenderness. A sample of dialysate reveals WBC 400/μL with 80% neutrophils. Empiric intraperitoneal antibiotic therapy should include:
A. Cefoxitin
B. Fluconazole
C. Metronidazole
D. Vancomycin
E. Voriconazole
IV-25. A 77-year-old man presents to the hospital with 1 week of fever, chills, nausea, and right upper quadrant pain. His temperature is 39°C, and he appears toxic. His blood pressure is 110/70 mmHg, heart rate is 110 beats/min, and respiratory rate is 22 breaths/min with room air O2 saturation 92%. He
has diminished breath sounds at the right base and diffuse tenderness in the right upper quadrant. He has a history of cholelithiasis but has declined elective cholecystectomy. His CT scan of the abdomen is shown in Figure IV-25A. Which of the following statements regarding his condition or therapy is true?

FIGURE IV-25A
A. Concomitant bacteremia is rare (<10%).
B. He should receive empiric antibiotics targeting Candida species.
C. He should receive empiric antibiotics targeting anaerobic organisms.
D. He should undergo percutaneous drainage.
E. His serum alkaline phosphatase is most likely normal.
IV-26. A 41-year-old man with hepatitis C–associated ascites presents with acute abdominal pain. Physical examination is notable for temperature of 38.3°C, heart rate of 115 beats/min, blood pressure of 88/48 mmHg, respiratory rate of 16 breaths/min, and oxygen saturation of 99% on room air. The patient is in moderate discomfort and is lying still. He is alert and oriented. His lungs are clear. Cardiac examination is unremarkable. His abdomen is diffusely tender with distant bowel sounds, mild guarding, and no rebound tenderness. Laboratory studies reveal a leukocyte count of 11,630/μL with 94% neutrophils, hematocrit of 29%, and platelet count of 24,000/μL. Paracentesis reveals 658 PMNs/μL, total protein of 1.2 g/dL, and glucose of 24 mg/dL and Gram stain showing gram-negative rods, gram-positive cocci in chains, gram-positive rods, and yeast forms. All of the following are indicated EXCEPT:
A. Abdominal radiograph
B. Broad-spectrum antibiotics
C. Drotrecogin alfa
D. Intravenous fluid
E. Surgical consultation
IV-27. Enteric pathogens can produce diarrheal illness through a variety of mechanisms that lead to specific clinical characteristics. All of the following are characteristics of diarrhea caused by Vibrio cholerae EXCEPT:
A. Disease localized to the proximal small intestine
B. Fecal leukocytes
C. Fecal lactoferrin
D. Toxin production
E. Watery diarrhea
IV-28. A 46-year-old woman travels to a rural area of Guatemala. Three days after arrival, she develops watery diarrhea with severe abdominal cramping. She reports two unformed stools daily for the past 2 days. She has noticed no blood in the stool and has not experienced a fever. What is the most likely cause of the patient’s illness?
A. Campylobacter jejuni
B. Enterotoxigenic Escherichia coli
C. Giardia lamblia
D. Norovirus
E. Shigella spp.
IV-29. For the case above, which of the following treatments would you recommend?
A. Azithromycin 10 mg/kg on day 1 with 5 mg/kg on days 2 and 3 if the diarrhea persists
B. Ciprofloxacin 500 mg three times daily for 5 days
C. Ciprofloxacin 750 mg once
D. Loperamide 4 mg once followed by 2 mg after passage of each unformed stool
E. Oral rehydration therapy only
IV-30. Two hours after attending a company picnic, many individuals who attended the picnic develop an acute gastrointestinal illness. Food poisoning caused by Staphylococcus aureus is suspected. All of the following characteristics would be a common feature of food poisoning due to this organism EXCEPT:
A. Abdominal cramping
B. Diarrhea
C. Fever
D. Vomiting
IV-31. You are the on-call physician practicing in a suburban community. You receive a call from a 28-year-old woman with a past medical history significant for sarcoidosis who is currently taking no medications. She is complaining of an acute onset of crampy diffuse abdominal pain and multiple episodes of emesis that are nonbloody. She has not had any lightheadedness with standing or loss of
consciousness. When questioned further, the patient states that her last meal was 5 hours previously, when she joined her friends for lunch at a local Chinese restaurant. She ate from the buffet, which included multiple poultry dishes and fried rice. What should you do for this patient?
A. Ask the patient to go to the nearest emergency department for resuscitation with IV fluids.
B. Initiate antibiotic therapy with azithromycin.
C. Reassure the patient that her illness is self-limited and no further treatment is necessary if she
can maintain adequate hydration.
D. Refer the patient for CT to assess for appendicitis.
E. Refer the patient for admission for IV vancomycin and ceftriaxone because of her
immunocompromised state resulting from sarcoidosis.
IV-32. Which of the following is a common manifestation of Clostridium difficile infection?
A. Fever
B. Nonbloody diarrhea
C. Adynamic ileus
D. Recurrence after therapy
E. All of the above
IV-33. All of the following patients should be treated for Clostridium difficile infection EXCEPT:
A. A 57-year-old nursing home resident with diarrhea for 2 weeks and pseudomembranes found on
colon-oscopy with no evidence of toxin A or B in the stool
B. A 63-year-old woman with fever, leukocytosis, adynamic ileus, and a positive PCR for C.
difficile in the stool
C. A 68-year-old woman with recent course of antibiotics admitted to the medical intensive care
unit after presentation to the emergency department with abdominal pain and diarrhea. She was found
to have severe abdominal tenderness with absent bowel sounds, systemic hypotension, and colonic
wall thickening on CT of the abdomen.
D. A 75-year-old woman who received recent therapy with amoxicillin for an upper respiratory
tract infection and now has two loose bowel movements per day for the past 3 days
IV-34. A 78-year-old woman with dementia has been living in a nursing home for 5 years. She was been seen by her primary care provider for evaluation of diarrhea 4 weeks ago. At that time, a stool sample was positive by PCR for Clostridium difficile, and she was treated with oral metronidazole with some improvement in her symptoms. However, she has had five loose bowel movements per day starting 4 days ago and now has abdominal tenderness. Stool PCR remains positive. Which of the following is the most appropriate therapy?
Date: 2016-04-22; view: 1666
| <== previous page | | | next page ==> |
| Men »5D ff Alncan Àäàèãî *ti or 4 page | | | ÀÌìÉÀæDVT, Jeep venous [Û)ÛêÐÅ, pulmonary embolism. 2 page |