
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
TABLE 1-149 Physiologic Characteristics of the Various Forms of Shock 4 page
II-29. The answer is E. (Chap. 79) Based on the American Psychiatric Association’s practice guidelines, inpatient treatment or partial hospitalization is indicated for patients whose weight is less than 75% of expected for age and height, who have severe metabolic disturbances (e.g., electrolyte disturbances, bradycardia, hypotension), or who have serious concomitant psychiatric problems (e.g., suicidal ideation, substance abuse). There should be a low threshold for inpatient treatment if there has been
rapid weight loss or if weight is less than 80% of expected. Amenorrhea, exaggeration of food intake, and fear of gaining weight are part of the diagnostic criteria for AN, and purging is not uncommon in this population. Weight restoration to 90% of predicted weight is the goal of nutritional therapy.
II-30. The answer is D. (Chap. 79) Approximately 25–50% of patients with anorexia nervosa (AN) recover fully with few physiologic or psychological sequelae. However, many patients have persistent difficulties with weight maintenance, depression, and eating disturbances. Approximately 5% of patients with AN die per decade, usually due to the physical effects of chronic starvation or from suicide. Virtually all of the physiologic derangements associated with AN will improve with weight gain. One exception is the loss of bone mass, which may not recover fully when AN occurs during adolescence (i.e., during peak bone mass formation). Psychological health also improves with successful treatment, although these patients remain at risk for depression, recurrence, and development of bulimia nervosa.
II-31. The answer is E. (Chap. 80) Involuntary weight loss (IWL) is a frequent finding in older individuals, affecting more than 25% of frail individuals older than 65 years. Clinically important weight loss is defined as a loss of more than 5% of body weight or more than 5 kg over the course of 6– 12 months. In older individuals, weight loss is associated with hip fracture, pressure ulcers, decreased functional status, and death. There are many causes of IWL, with the most common categories being malignancy, chronic inflammatory or infectious disease, metabolic disorders, and psychiatric disorders. In older individuals, it is also important to consider neurologic disorders, including stroke leading to dysphagia, progressive vision loss, and dementia. IWL can be one of the earliest manifestations of Alzheimer’s disease. An under-recognized cause of IWL is lack of access to food or inability to pay for food. When evaluating an individual for IWL, a complete physical examination, including a dental examination, should be performed to assess for obvious physical causes that would lead to weight loss. Medications may also lead to changes in appetite or weight loss. Patients should undergo age-appropriate cancer screening. In older individuals, a Mini-Mental State Examination, Mini-Nutritional Assessment, and assessment of performance of activities of daily living may be helpful. It may also be useful to observe the patient’s eating. Depression in the elderly may also present with loss of appetite and should be assessed. Laboratory studies could include a complete blood count, comprehensive metabolic panel, thyroid function tests, and erythrocyte sedimentation rate and C-reactive protein. HIV testing is indicated if risk factors are identified.
SECTION III
Oncology and Hematology
QUESTIONS
DIRECTIONS: Choose the one best response to each question. III-1. For each patient choose the most likely peripheral blood smear: (See Figure III-1)
| PI "6 |
0îÎë¹Ø
| *tasra |
| î |
t¹

|
| \$ |
| æ |
| Î |
| ) |
| ™9* |
| U |


|
Ft ×Ê
Ï

FIGURE III-1 (see Color Atlas)
1. A 22-year-old man with a hematocrit of 17%. He has sickle cell disease and is admitted with a vaso-occlusive crisis after an upper respiratory illness.
2. A 36-year-old woman with a hematocrit of 32%. She had a splenectomy 5 years ago after a motor vehicle crash.
3. A 55-year-old man with a hematocrit of 28%. He has advanced alcoholic liver disease with cirrhosis and is awaiting liver transplantation.
4. A 64-year-old woman with a hematocrit of 28%. She has heme-positive stool and a 2-cm
adenomatous colonic polyp at colonoscopy.
5. A 72-year-old man a hematocrit of 33%. Four years ago, he received a mechanical prosthetic
aortic valve because of aortic stenosis caused by a congenital bicuspid valve.
III-2. A 39-year-old woman is evaluated for anemia. Her laboratory studies reveal a hemoglobin of 7.4 g/dL, hematocrit of 23.9%, mean corpuscular volume of 72 fL, mean cell hemoglobin of 25 pg, and mean cell hemoglobin concentration of 28%. The peripheral smear is shown in Figure III-2. Which of the following tests is most likely to be abnormal in this patient?

FIGURE III-2 (see Color Atlas)
A. Ferritin
B. Haptoglobin
C. Hemoglobin electrophoresis
D. Glucose-6-phosphate dehydrogenase
E. Vitamin B12
III-3. A 62-year-old man is evaluated for anemia. He has a hemoglobin of 9.0 g/dL (normal hemoglobin value, 15 g/dL), hematocrit of 27.0% (normal hematocrit, 45%), mean cell volume of 88 fL, mean cell hemoglobin of 28 pg, and mean cell hemoglobin concentration of 30%. On peripheral blood smear, polychromatophilic macrocytes are seen. The reticulocyte count is 9%. What is the reticulocyte production index?
A. 0.54
B. 1.67
C. 2.7
D. 4.5
E. 5.4
III-4. You are asked to review the peripheral blood smear from a patient with anemia ( Figure III-4). Serum lactate dehydrogenase is elevated, and there is hemoglobinuria. This patient is likely to have which physical examination finding?
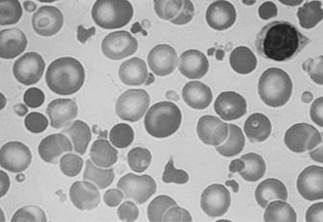
FIGURE III-4 (see Color Atlas)
A. Goiter
B. Heme-positive stools
C. Mechanical second heart sound
D. Splenomegaly
E. Thickened calvarium
III-5. In general, which of the following is the greatest risk factor for the development of cancer?
A. Age
B. Alcohol use
C. Cigarette smoking
D. Female sex
E. Obesity
III-6. Among women younger than 60 years of age who die from cancer, which of the following is the most common primary organ of origin?
A. Breast
B. Cervix
C. Colon
D. Bone marrow
E. Lung
III-7. A 68-year-old woman is diagnosed with stage II breast cancer. She has a history of severe chronic obstructive pulmonary disease with an FEV1 of 32% predicted, coronary artery disease with prior
stenting of the left anterior descending artery, peripheral vascular disease, and obesity. She continues to smoke 1 to 2 packs of cigarettes every day. She requires oxygen at 2 L/min continuously and is functionally quite limited. She currently is able to attend to all of her activities of daily living, including showering and dressing. She retired from her work as a waitress 10 years previously because of her lung disease. At home, she does attend to some of the household chores but is not able to use a vacuum. She goes out once or twice weekly to run typical errands and drives. She feels short of breath with most of these activities and often uses a motorized chart when out and about. How would you categorize her
performance status and prognosis for treatment taking this into consideration?
A. She has an Eastern Cooperative Oncology Group (ECOG) grade of 1 and has a good prognosis
with appropriate therapy.
B. She has an ECOG grade of 2 and has a good prognosis with appropriate therapy.
C. She has an ECOG grade of 3 and has a good prognosis with appropriate therapy.
D. She has an ECOG grade of 3 and has a poor prognosis despite therapy.
E. She has an ECOG grade of 4 and has a poor prognosis that precludes therapy.
III-8. Which of the following tumor markers is appropriately matched with the cell type cancer and can be followed during treatment as an adjunct to assess disease burden?
A. CA-125—Colon cancer
B. Calcitonin—Follicular carcinoma of the thyroid
C. CD30—Hairy cell leukemia
D. Human chorionic gonadotropin—Gestational trophoblastic disease
E. Neuron-specific enolase—Non–small cell carcinoma of the lung
III-9. Which of the following statements regarding current understanding of the genetic changes that must occur for a cell to become cancerous is TRUE?
A. Caretaker genes determine when a cell enters into a replicative phase and must acquire
mutations to allow unregulated cell growth.
B. For a cell to become cancerous, it is estimated that a minimum of 20 mutations must occur.
C. For a tumor suppressor gene to become inactivated and allow unregulated cell growth, both
copies of the gene must have mutations.
D. Oncogenes act in an autosomal recessive fashion.
E. Within a cancer, there are generally two to five cells of origin.
III-10. All the following conditions are associated with an increased incidence of cancer EXCEPT:
A. Down syndrome
B. Fanconi’s anemia
C. von Hippel–Lindau syndrome
D. Neurofibromatosis
E. Fragile X syndrome
III-11. Cancer therapy is increasingly personalized with targeted small molecule therapies that are directed against specific signal transduction pathways that are commonly activated in a particular cell type of cancer. Which of the following therapies is correctly matched with its molecular target?
A. Bevacizumab—EGFR
B. Erlotinib—VEGF
C. Imatinib—Bcr-Abl
D. Rituximab—CD45
E. Sunitinib—RAF
III-12. Which of the following defines the term epigenetics?
A. Changes that alter the pattern of gene expression caused by mutations in the DNA code
B. Changes that alter the pattern of gene expression that persist across at least one cell division but
are not caused by changes in the DNA code
C. Irreversible changes of the chromatin structure that regulates gene transcription and cell
proliferation without permanent alteration of the DNA code
III-13. Which of the following patients with metastatic disease is potentially curable by surgical resection?
A. A 24-year-old man with a history of osteosarcoma of the left femur with a 1-cm metastasis to his
right lower lobe referred for right lower lobectomy
B. A 56-year-old woman with a history of colon cancer with three metastases to the left lobe of the
liver referred for left hepatic lobectomy
C. A 72-year-old man with metastatic prostate cancer to several vertebrae referred for orchiectomy
D. All of the above
E. None of the above
III-14. You are studying a new chemotherapeutic agent for use in advanced colorectal carcinoma and have completed a phase II clinical trial. Which of the following factors indicates that the drug is suitable for study in a phase III clinical trial?
A. Complete response rates of 10% to 15%
B. Increased disease-free survival rates by 1 month
C. Increased overall survival by 1 month
D. Partial response rate of 20% to 25%
E. Partial response rates of 50% or more
III-15. Match the following chemotherapeutic agents with their mechanisms of action:.

III-16. A 48-year-old woman with stage III breast cancer is undergoing chemotherapy with a regimen that includes doxorubicin. She presents 8 days after her last treatment to the emergency department with a fever of 104.1°F (40.1°C). She has chills, rigors, and a headache. Her chest radiograph, urinalysis, and tunneled intravenous catheter site show no obvious evidence of infection. Her white blood cell count upon presentation is 500/μL (0% neutrophils, 50% monocytes, 50% lymphocytes). Blood cultures are drawn peripherally and through the catheter. What is the next step in the treatment of this patient?
A. Broad-spectrum antibiotics with ceftazidime and vancomycin
B. Broad-spectrum antibiotics with ceftazidime, vancomycin, and voriconazole
C. Granulocyte-macrophage colony-stimulating factor after subsequent cycles of chemotherapy only
D. Granulocyte-macrophage colony-stimulating factor now and after subsequent cycles of
chemotherapy
E. A and C
F. A and D
III-17. What is the most common side effect of chemotherapy?
A. Alopecia
B. Diarrhea
C. Febrile neutropenia
D. Mucositis
E. Nausea with or without vomiting
III-18. A 24-year-old woman is seen in follow-up 12 months after an allogeneic stem cell transplant for acute myeloid leukemia. She is doing well without evidence of recurrent disease but has had manifestations of chronic graft-versus-host disease. She should be administered all of the following vaccines EXCEPT:
A. Diphtheria–tetanus
B. Influenza
C. Measles, mumps, and rubella
D. Poliomyelitis via injection
E. 23-Valent pneumococcal polysaccharide
III-19. A 66-year-old woman has chronic lymphocytic leukemia with a stable white blood cell count of between 60,000 and 70,000/μL. She is currently hospitalized with pneumococcal pneumonia. This is the patient’s third episode of pneumonia within the past 12 months. What finding on laboratory testing would be most likely in this patient?
A. Granulocytopenia
B. Hypogammaglobulinemia
C. Impaired T-cell function with normal T-lymphocyte counts
D. Low CD4 count
E. No specific abnormality is expected.
III-20. A 63-year-old man is treated with chemotherapy for stage IIIB adenocarcinoma of the lung with paclitaxel and carboplatin. He presents for evaluation of a fever of 38.3°C (100.9°F). He is found to have erythema at the exit site of his tunneled catheter, although the tunnel itself is not tender or red. Blood cultures are negative at 48 hours. His neutrophil count is 1,550/μL. What is the best approach to the management of this patient?
A. Removal of catheter alone
B. Treatment with ceftazidime and vancomycin
C. Treatment with topical antibiotics at the catheter site
D. Treatment with vancomycin alone
E. Treatment with vancomycin and removal of catheter
III-21. A 48-year-old woman presents to her physician with a complaint of an enlarging mole on her right lower extremity. She had noticed the area about 1 year previously and believes it has enlarged. She also notes that it recently has become itchy and occasionally bleeds. On physical examination, the lesion is located on the right mid-thigh. It measures 7.5 × 6 mm with irregular borders and a variegated hue with some areas appearing quite black. A biopsy confirms nodular melanoma. Which of the following is the best predictor of metastatic risk in this patient?
A. Breslow thickness
B. Clark level
C. Female gender
D. Presence of ulceration
E. Site of lesion
III-22. A 53-year-old man with a history of superficial spreading melanoma is diagnosed with disease metastatic to the lungs and bones. Genetic testing confirms the presence of the BRAF V600E mutation. What do you recommend for treatment of this patient?
A. Dacarbazine
B. Hospice care
C. Interleukin-2
D. Ipilimumab
E. Vemurafenib
III-23. A 65-year-old man presents to his primary care physician complaining of a hoarse voice for 6 months. He smokes 1 pack of cigarettes daily and drinks at least a six pack of beer daily. His physical examination reveals a thin man with a weak voice in no distress. No stridor is heard. The head and neck examination is normal. No cervical lymphadenopathy is present. He is referred to otolaryngology where a laryngeal lesion is discovered. Biopsy reveals squamous cell carcinoma. On imaging, the mass measures 2.8 cm. No suspicious lymphadenopathy is present on PET imaging. What is the best choice of therapy in this patient?
A. Concomitant chemotherapy and radiation therapy
B. Chemotherapy alone
C. Radiation therapy alone
D. Radical neck dissection alone
E. Radical neck dissection followed by concomitant chemotherapy and radiation
III-24. Which of the following statements is true with regard to the solitary pulmonary nodule?
A. A lobulated and irregular contour is more indicative of malignancy than a smooth one.
B. About 80% of incidentally found pulmonary nodules are benign.
C. Absence of growth over a period of 6 to 12 months is sufficient to determine if a solitary
pulmonary nodule is benign.
D. Ground-glass nodules should be regarded as benign.
E. Multiple nodules indicate malignant disease.
III-25. A 64-year-old man seeks evaluation for a solitary pulmonary nodule that was found incidentally. He had presented to the emergency department for shortness of breath and chest tightness. A CT pulmonary angiogram did not show any evidence of pulmonary embolism. However, a 9-mm nodule is seen in the periphery of the left lower lobe. No enlarged mediastinal lymph nodes are present. He is a current smoker of 2 packs of cigarettes daily and has done so since the 16 years of age. He generally reports no functional limitation related to respiratory symptoms. His FEV1 is 88% predicted, FVC is
92% predicted, and diffusion capacity is 80% predicted. He previously had a normal chest x-ray 3 years previously. What is the next best step in the evaluation and treatment of this patient?
A. Perform a bronchoscopy with biopsy for diagnosis.
B. Perform a combined PET and CT to assess for uptake in the nodule and assess for lymph node
metastases.
C. Perform a follow-up CT scan in 3 months to assess for interval growth.
D. Refer the patient to radiation oncology for stereotactic radiation of the dominant nodule.
E. Refer the patient to thoracic surgery for video-assisted thoracoscopic biopsy and resection of
lung nodule if malignancy is diagnosed.
III-26. A 62-year-old man presents to the emergency department complaining of a droopy right eye and blurred vision for the past day. The symptoms started abruptly, and he denies any antecedent illness. For the past 4 months, he has been complaining of increasing pain in his right arm and shoulder. His primary care physician has treated him for shoulder bursitis without relief. His medical history is significant for COPD and hypertension. He smokes 1 pack of cigarettes daily. He has chronic daily sputum production and has stable dyspnea on exertion. On physical examination, he has right eye ptosis with unequal pupils. On the right, his pupil is 2 mm and not reactive; on the left, the pupil is 4 mm and reactive. However, his ocular movements appear intact. His lung fields are clear to auscultation. On extremity examination, there is wasting of the intrinsic muscles of the hand. Which of the following would be most likely to explain the patient’s constellation of symptoms?
A. Enlarged mediastinal lymph nodes causing occlusion of the superior vena cava
B. Metastases to the midbrain from small cell lung cancer
C. Paraneoplastic syndrome caused by antibodies to voltage-gated calcium channels
D. Presence of a cervical rib on chest radiography
E. Right apical pleural thickening with a mass-like density measuring 1 cm in thickness
III-27. A 55-year-old man presents with superior vena cava syndrome and is diagnosed with small cell lung cancer. Which of the following tests are indicated to properly stage this patient?
A. Bone marrow biopsy
B. CT scan of the abdomen
C. CT or MRI of the brain with intravenous contrast
D. Lumbar puncture
E. B and C
F. All of the above
III-28. As an oncologist you are considering treatment options for your patients with lung cancer, including small molecule therapy targeting the epidermal growth factor receptor (EGFR). Which of the following patients is most likely to have an EGFR mutation?
A. A 23-year-old man with a hamartoma
B. A 33-year-old woman with a carcinoid tumor
C. A 45-year-old woman who has never smoked with an adenocarcinoma
D. A 56-year-old man with a 100 pack-year history of tobacco with small cell lung carcinoma
E. A 76-year-old man with squamous cell carcinoma and a history of asbestos exposure
III-29. Given that most individuals with lung cancer present with advanced disease and have a high mortality, much research has investigated methods for early detection of lung cancer. Which of the following approaches is most likely to impact disease-related mortality from lung cancer?
A. Carefully design and implement low-dose chest CT screening in individuals with greater than 30
pack years of cigarette smoking
B. Continue annual screening with a chest x-ray for individuals with greater than 30 pack years of
cigarette smoking
C. Do not recommend any screening because 30 years of research has not demonstrated any effect
on mortality from lung cancer
D. Offer screening with low-dose CTs to all current or former smokers
E. Offer screening with combined PET and CT to individuals with greater than 30 pack years of
tobacco use
III-30. A 34-year-old woman is seen by her internist for evaluation of right breast mass. This was noted approximately 1 week ago when she was showering. She has not had any nipple discharge or discomfort. She has no other medical problems. On examination, her right breast has a soft 1 cm × 2 cm mass in the right upper quadrant. There is no axillary lymphadenopathy present. The contralateral breast is normal. The breast is reexamined in 3 weeks, and the same findings are present. The cyst is aspirated, and clear fluid is removed. The mass is no longer palpable. Which of the following statements is true?
A. Breast MRI should be obtained to discern for residual fluid collection.
B. Mammography is required to further evaluate the lesion.
C. She should be evaluated in 1 month for recurrence.
D. She should be referred to a breast surgeon for resection.
E. She should not breastfeed any more children.
III-31. Which of the following women has the lowest risk of breast cancer?
A. A woman with menarche at 12 years, first child at 24 years, and menopause at 47 years
B. A woman with menarche at 14 years, first child at 17 years, and menopause at 52 years
C. A woman with menarche at 16 years, first child at 17 years, and menopause at 42 years
D. A woman with menarche at 16 years, first child at 32 years, and menopause at 52 years
E. They are all equal
III-32. Which of the following tumor characteristics confers a poor prognosis in patients with breast cancer?
A. Estrogen receptor positive
B. Good nuclear grade
C. Low proportion of cells in S-phase
D. Overexpression of erbB2 (HER-2/neu)
E. Progesterone receptor positive
III-33. A 56-year-old man presents to a physician with weight loss and dysphagia. He feels that food gets stuck in his mid-chest such that he no longer is able to eat meats. He reports his diet consists primarily of soft foods and liquids. The symptoms have progressively worsened over 6 months. During this time, he has lost about 50 lb. He occasionally gets pain in his mid-chest that radiates to his back and also occasionally feels that he regurgitates undigested foods. He does not have a history of gastroesophageal reflux disease. He does not regularly seek medical care. He is known to have hypertension but takes no medications. He drinks 500 cc or more of whiskey daily and smokes 1.5 packs of cigarettes per day. On physical examination, the patient appears cachectic with temporal wasting. He has a body mass index of 19.4 kg/m2. His blood pressure is 198/110 mm Hg, heart rate is 110 beats/min, respiratory rate is 18 breaths/min, temperature is 37.4°C (99.2°F), and oxygen saturation is 93% on room air. His pulmonary examination shows decreased breath sounds at the apices with scattered expiratory wheezes. His cardiovascular examination demonstrates an S4 gallop with a hyperdynamic precordium. A regular tachycardia is present. Blood pressures are equal in both arms. Liver span is not enlarged. There are no palpable abdominal masses. What is the most likely cause of the patient’s presentation?
A. Adenocarcinoma of the esophagus
B. Ascending aortic aneurysm
C. Esophageal stricture
D. Gastric cancer
E. Squamous cell carcinoma of the esophagus
III-34. A 64-year-old woman presents with complaints of a change in stool caliber for the past 2 months. The stools now have a diameter of only the size of her fifth digit. Over this same period, she feels she has to exert increasing strain to have a bowel movement and sometimes has associated abdominal cramping. She often has blood on the toilet paper when she wipes. During this time, she has lost about 20 lb. On physical examination, the patient appears cachectic with a body mass index of 22.5 kg/m2. The abdomen is flat and nontender. The liver span is 12 cm to percussion. On digital rectal examination, a mass lesion is palpated approximately 8 cm into the rectum. A colonoscopy is attempted, which demonstrates a 2.5-cm sessile mass that narrows the colonic lumen. The biopsy confirms adenocarcinoma. The colonoscope is not able to traverse the mass. A CT scan of the abdomen does not show evidence of metastatic disease. Liver function test results are normal. A carcinoembryonic antigen level is 4.2 ng/mL. The patient is referred for surgery and undergoes rectosigmoidectomy with pelvic lymph node dissection. Final pathology demonstrates extension of the primary tumor into the muscularis propria but not the serosa. Of 15 lymph nodes removed, two are positive for tumor. What do you
recommend for this patient after surgery?
A. Chemotherapy with a regimen containing 5-fluorouracil
B. Complete colonoscopy within 3 months
C. Measurement of CEA levels at 3-month intervals
D. Radiation therapy to the pelvis
E. All of the above
III-35. A healthy 62-year-old woman returns to your clinic after undergoing routine colonoscopy. Findings included two 1.3-cm sessile (flat-based), villous adenomas in her ascending colon that were removed during the procedure. What is the next step in management?
A. Colonoscopy in 3 years
B. Colonoscopy in 10 years
C. CT scan of the abdomen
D. Partial colectomy
E. Reassurance
III-36. Which of the following should prompt investigation for hereditary nonpolyposis colon cancer screening in a 32-year-old man?
A. Father, paternal aunt, and paternal cousin with colon cancer with ages of diagnosis of 54, 68,
and 37 years, respectively
B. Innumerable polyps visualized on routine colonoscopy
C. Mucocutaneous pigmentation
D. New diagnosis of ulcerative colitis
E. None of the above
III-37. All of the following statements regarding pancreatic cancer are true EXCEPT:
A. Alcohol consumption is not a risk factor for pancreatic cancer.
B. Cigarette smoking is a risk factor for pancreatic cancer.
C. Despite accounting for fewer than 5% of malignancies diagnosed in the United States, pancreatic
cancer is the fourth leading cause of cancer death.
Date: 2016-04-22; view: 961
| <== previous page | | | next page ==> |
| TABLE 1-149 Physiologic Characteristics of the Various Forms of Shock 3 page | | | TABLE 1-149 Physiologic Characteristics of the Various Forms of Shock 5 page |