
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Congenital Heart Disease
Definition:-
- Anomalies of heart and large vessels development due to embriogenesis disturbances during 2-8th weeks of pregnancy
Epidemiology :-
- Frequency - 1%
- 50-70 % die before 1 year of age (if without surgery)
- Only ½ of cases are diagnosed in maternity house; 93% - before 1st year
- More than 40 defects are described; 8 are most common (80%)
Most common defects :-
- Ventricular septal defect (VSD)
- Atrial septal defect (ASD)
- Patent ductusarteriosus (PDA)
- Coarctation of aorta (CA)
- Stenosis of aorta (SA)
- Transposition of magistral vessels (TMV)
- Fallot’s tetralogy (FT)
Etiology – 1:-
- Viral infections (rubella, URIs, mumps, chickenpox)
- Radioactive rays
- Drugs (thalidomide)
- Toxicosis of pregnancy
- Starving
- Polyhypovitaminosis
Etiology – 2:-
- Some diseases of pregnancy (diabetes, heart diseases)
- Chromosomal diseases (Down’s syndrome, Marfan’s syndrome, Turner’s syndrome…)
- Mother’s age over 35 years
- Maternalalcoholconsumption
- Family history of a cardiac or noncardiac defect
Classification – I:-
- With left-to-right shunting (↑ pulmonary circulation)
- With right-to-left shunting (↓ pulmonary circulation)
- Without shunting
With left-to-right shunting:-
- Ventricular septal defect
- Atrial septal defect
- Patent ductusarteriosus
With right-to-left shunting:-
- Transposition of magistral vessels
- Fallot’s tetralogy
- Left heart hypoplasia
Without shunting:-
- Coarctation of aorta
- Stenosis of aorta
- Stenosis of pulmonary artery
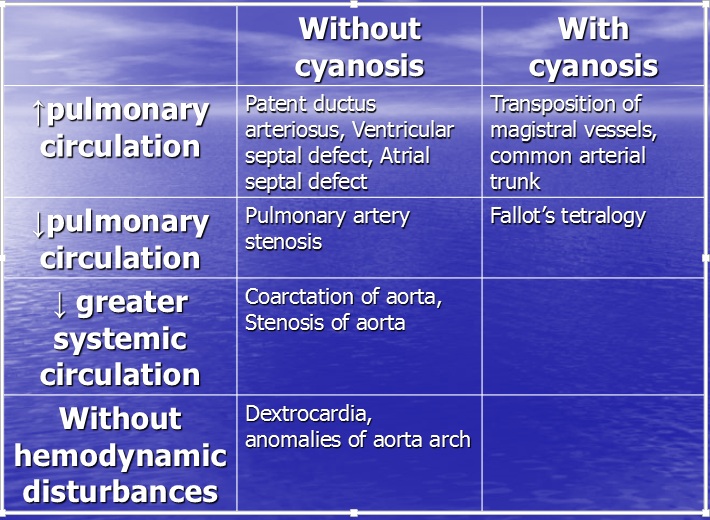
Classification – II:-
- With increase of pulmonary circulation
- With decrease of pulmonary circulation With decrease of greater systemic circulation
- Without hemodynamic disturbances
- ___________
- With or without cyanosis
Echocardiography:-
- 3-dimensional (3D) echocardiographic images with a Doppler system with superimposing a color-coded direction and velocity of blood flow on the real-time images
Ventricular septal defect:-
- Most common: 17-30 %
- Size:0.1 cm – 3 cm
- Localization: in membranous or muscular part
- Delayed diagnosis: first months pulmonary pressure is higher → no cardiac murmur
Ventricular septal defect:-
- Small VSD: no significant hemodynamic derangement; loud murmur; can close spontaneously (in muscle segment)
- Large VSD: progressively leads to higher pulmonary resistance → irreversible pulmonary vascular changes, so-called Eisenmenger syndrome (reversal of shunt to right-to-left shunt)
Clinics:-
- Mild defect: recurrent upper respiratory infections, effort intolerance and fatigue
- Severe defect:
- Development deficit, failuretothrive
- CHF
- Pulmonary hypertension
Clinics in early infancy:-
- Dyspnea
- Feedingdifficulties
- Poorgrowth
- Profuseperspiration
- Recurrentpulmonaryinfections
- Cardiacfailure
Physical exam:-
- Rough pansystolic murmur in 3-4th intercostal space on the left border of sternum
- Accent of S2 over pulmonary artery (pulmonary hypertension)
- Left and right ventricular enlargement (palpable parasternal lift, laterally displaced apical impulse, widened heart borders)
ECG:-
- Small VSD → Normal
- Moderate VSD → signs of LV volume overload (deep Q and tall R waves with tall T waves in leads V5 and V6), LA overload (broad P wave), atrial fibrillation
- Severe VSD → right ventricular hypertrophy, with further progression - biventricular hypertrophy
Chest X-ray:-
- Small VSD → Normal
- Moderate VSD → Increased cardiac silhouette, increased pulmonary vascular markings
- Severe VSD → Markedly prominent main PA and adjacent vessels, RV hypertrophy
Medical management:-
- Increasedcalories of feedings
- Diuretics (furosemide 1-3 mg/kg/d )
- Captopril (0.1-0.3 mg/kg every 8 h) to reduce systemic and pulmonary afterload
- Digoxin (5-10 mcg/kg/d) - if diuresis and afterload reduction do not relieve symptoms adequately.
SurgicalCare:-
- Transcatheterclosure
- Surgicalclosure
- Indicationsforsurgicalrepair:
- Uncontrolled CHF
- Large, asymptomatic defects associated with elevated PA pressure
- Pulmonary to systemic flow greater than 2:1.
- Prolapseofanaorticvalve
Complications:-
- Eisenmengercomplex
- Secondaryaorticinsufficiency
- Aorticregurgitation
- RV outflowtractobstruction
- Subaorticobstruction
- Infective endocarditis (antibiotic prophylaxis with dental or surgical procedures)
Prognosis:-
- 25 % - spontaneous closure (mostly during the first 2 years of life, can be in adults)
- 7% of infants with large defects and congestive heart failure - also spontaneous closure
- Among small defects, 80% of muscular VSDs closed and 35% of membranous
- 10 % - death during 1st year of life
- Mean life expectancy – 40 years
Atrial septal defect:-
- Frequency: 8-15 %
- Size:small – to complete absence
- Open oval window → no clinics (30% of adults)
- Diagnosis at 1st year – only 40% of cases
Clinics:-
- Rarelysymptomatic
- Decreasedexercisetolerance
- Large shunt → fatigue, dyspnea and arrhythmias
Physical exam:-
- Moderate systolic murmur in 2nd intercostal space on the left border of sternum
- Accent of S2 over pulmonary artery (pulmonary hypertension)
- Signs of cardiac enlargement
ECG:-
- Right ventricular hypertrophy (lengthened PR interval and incomplete right bundle branch block)
- Atrialenlargement(P wave)
Chest x-ray:-
- Prominentrightatrium
- Prominentmainpulmonaryartery
- Increased heart size and pulmonary vascularity
Complications:-
- Sinusnodedysfunction
- Pulmonaryvenousobstruction
- Atrialfibrillation
- Pulmonaryhypertension
- Pericardial effusion or post-pericardiotomy syndrome
Prognosis:-
- Poor if CHF at early age
- Mean life expectancy – 40 years
- Best time for surgery – 1st two decades of life
- No Px for septic endocarditis
Patent ductusarteriosus:-
- Frequency: 10-25 %
- Prematures: 50-80%
- Normal finding at 1st week of life
- Ductus between descending aorta and pulmonary artery bifurcation
Clinics:-
- Repeated respiratory infections
- Later – liver enlargement, cyanosis
- Growth retardation
- Septic endocarditis
- CHF
Physical exam:-
- Loud systolic or systolic-diastolic murmur in the 2nd intercostal space left from sternum
- 1st sound accent over pulmonary artery
- Murmur diminishes at deep breath-in
- Murmur disappears with pulmonary hypertension → appears again with shift reverse
Chest X-ray:-
- LV enlargement; later + RV enlargement
- Prominent pulmonary vessels
Management:-
- Can be closed with indometacin prescription (PG E2 & I2 synthesis inhibitor) – 0.1 mg/kg q8h IV first 8-14 days of life
- Surgery best after 6 months but before severe pulmonary hypertension
Prognosis:-
- Many defects will spontaneously close before 6 mo of age
- Without surgery mortality is 20%
- Mean life expectancy is 35 years
Coarctation of aorta:-
- 5-8% ofallcongenitalheartdefects
- May occur as isolated defect or in association bicuspid aortic valve, ventricular septal defect and others
Clinics:-
- Infants – CHF (acute afterload increase after ductusarteriosus closure)
- Older children – hypertension (enough time for collaterals development)
- Left ventricle overwork → increased wall stress and compensatory ventricular hypertrophy
Physical exam:-
- Blood pressure discrepancies between upper and lower extremities
- Reduced or absent lower extremity pulses
- Differential cyanosis (pink upper extremities with cyanotic lower extremities) - rare
- Murmur: nonspecific, under the left scapula
Chest X-ray:-
- Early onset of CoA: cardiomegaly, pulmonary edema, and other signs of CHF.
- Late onset of CoA: cardiomegaly, arch indentation in the area of the coarctation, and rib notching
ECG:-
- Early onset of symptoms: RV rather than LV hypertrophy and evidence of ischemia.
- Late onset of symptoms: LV hypertrophy and signs of LV ischemia or strain.
Other tests:-
- Preductal and postductal pulse oximetry readings
- Cardiac catheterization (evaluation and possible balloon aortoplasty)
Management:-
- Prostaglandin E1 (0.05-0.15 mcg/kg/min) IV to open the ductusarteriosus
- Treatment of hypertension (beta-blockers and vasodilators)
- Treatment of CHF and shock in infants
Surgery:-
- End-to-endanastomosis
- Patchaortoplasty
- Left subclavian flap aortoplasty (left subclavian artery is brought back toward the left carotid artery to enlarge an area of transverse arch hypoplasia)
Complications:-
- Hypertension
- Intracranialhemorrhageand aneurysms
- Aorticruptureordissection
- CHF
- Recurrentcoarctationafter surgery
- Aortic aneurythm
- Paralysis(spinal cord ischemia)
- Cardiomyopathy
Prognosis:-
- Meanlife expectancy is 35 years
- Without surgery 1-st year mortality is 25%
- Requires bacterialendocarditisprophylaxis
Transposition of magistral vessels:-
- Aorta comes from RV and pulmonary artery comes from LV → 2 separated circulations
- No disturbance of fetal circulation
- Postnatal life is only possible with blood shunts (VSD, ASD, PDA)
Clinics:-
- Early total cyanosis from birth, not responsive to oxygen
- Tachycardia, tachypnoe, decreased BP
- Developmental deficit
- CHF by 1st-2nd month of life
Physical exam:-
- Murmurs – due to other defects (VSD, ASD, PDA)
- Cardiac borders widening
Chest X-ray and ECG:-
- Signs of RV (or both) hypertrophy
Management:-
- Urgent surgery!
Prognosis:-
- 95% die during 1st year of life without surgery
- Mean life expectancy is 3 months
Fallot’s tetralogy:-
- Most common among cyanotic heart defects
- Right-to-left shunt
Defects of TOF:-
- Ventricularseptaldefect
- Dextrapositionoftheaorta
- Obstruction of the right ventricular outflow tract (PA stenosis)
- Rightventricularhypertrophy
- Pentade: + Atrial septal defect
- Triade: no VSD, shunt through Open oval fenestra
Clinics:-
- 4 phases:
- “Relative stable well-being”
- “Gray attacks”
- “Blue attacks”
- “Stabilization of the condition”
“Relative stable well-being”:-
- First 4-6 weeks of life
- PDA & Physiologic polycytemia → mild clinics and mild murmur (if any)
“Gray attacks”:-
- First 2-9 months of life
- Hypoxic attacks after physical strains (feeding, anxiety) – 20-25 times per day
- No cyanosis
- No complaints between attacks
- Failure to thrive
“Gray attacks” - Hypoxic attacks:-
- Sudden dyspnoe
- Grayish skin color
- Crying
- Short-period loss of consciousness
- Short-period seizures
“Blue attacks”:-
- 9 months – 3-5 years of life or all life long
- Systemic cyanosis first at attacks, then permanent
- Drumstick fingers
- Polycytemia
- Polyhlobulinemia
- Paresis and palsies (brain hemodynamics disturbances)
“Blue attacks” - Hypoxic attacks:-
- Involuntary position (knees at chest, older – squatting down): aortic pressure is increased → better shunt to pulmonary artery
- Cyanosis and dyspnea
“Stabilization of the condition”:-
- After 3-5 years:
- Permanent cyanosis, but without attacks
- Tachypnea at rest
- Murmus is less
- ECG, X-ray, Echo - worse
Physical exam:-
- Murmur of VSD
- Decreased 2nd sound over pulmonary artery
ECG:-
- Rightventricularhypertrophy
- Left ventricular overload and some left ventricular enlargement
- Right atrial enlargement may also be present
Chest X-ray:-
- Aneurysmally dilated central pulmonary arteries with otherwise normal peripheral pulmonary vascularity.
- Cardiomegaly results from dilation of the right ventricle, particularly its outflow tract (infundibulum)
- Appearance of “boot”
Management:-
- Attacks – position, oxygen, sedatives
- Surgery!
Prognosis:-
- Without surgery – 75% mortality before 2 years of age
Date: 2015-01-11; view: 1627
| <== previous page | | | next page ==> |
| What You See: Summary | | | COURT SYSTEM OF THE RUSSIAN FEDERATION |