
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
SURGICAL
Laparotomy is indicated in patients with peritonitis after rapid resuscitation. The first step is to assess the degree and extent of bowel viability. Free, foul smelling peritoneal fluid is a sign of advanced necrosis even if perforation has not occurred. Ischemic bowel has a characteristic appearance with loss of its normal sheen. It is dull, gray in color and flabby in tone without any peristalsis. Infarcted bowel is purplish black in color, often friable and perforated. In many cases the bowel ischemia will be so extensive and advanced that no further surgical treatment is undertaken and palliative care given. Where there is hope of sufficient bowel viability, revascularization should be performed before any bowel resection is considered. After successful revascularization, previously precarious segments of intestine may recover and resection of clearly ischemic bowel can then take place.
SMA embolectomy. The proximal portion of the SMA is dissected free from the surrounding fat and lymphatic tissue just as it emerges from the pancreatic neck into the base of the mesentery. Approximately 3 to 4 centimeters of artery is cleared, with care taken not to damage the branches. Heparin (5000 units) is given intravenously. A transverse arteriotomy is made and a 3F or 4F embolectomy catheter is passed proximally and distally to clear the embolus and reestablish vigorous pulsatile flow. If proximal flow cannot be established, SMA thrombosis is likely and reconstructive surgery will be required.
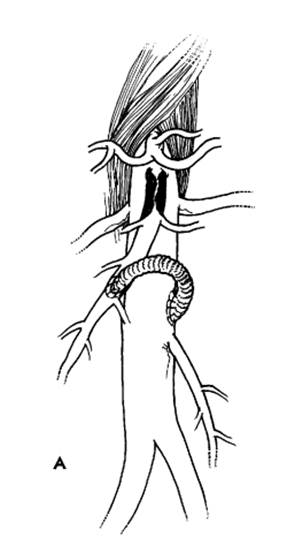

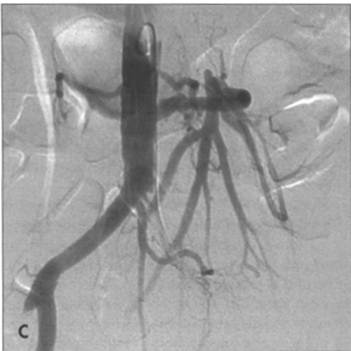
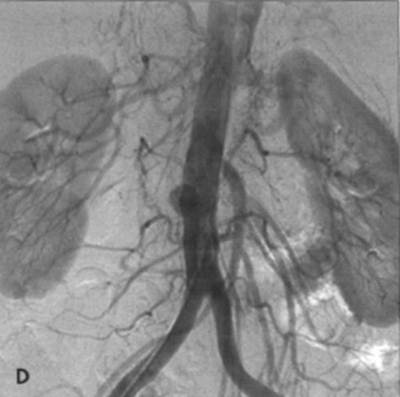
FIG. A - Schematic representation of revascularization of the SMA with: bypass taking care to avoid kinking and obs-
truction B - Or re-implantation of SMA into the aorta. C - Angiographic appearance of aorto-SMA bypass with vein graft.
There is co-existing left common iliac occlusion. D - Angiographic appearance of re-implanted SMA into aorta, which has
a smal l saccular aneurysm at the site of occluded vein graft (aortoceliac bypass).
Date: 2014-12-29; view: 1653
| <== previous page | | | next page ==> |
| Diagnosis | | | IS THERE A EUROPEAN ACCENT IN EURO DISNEYLAND? |