
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Tumours of lungs
Distinguish between bening and malignant tumours of lungs.Bening tumours are divided into 2 groups after localization (intrabronchial and intrapulmonar) and after a histological structure (epithelium are adenomas, papiloma, unepithelium, - gammartoma, lypoma, chondroma, myoma, neuroma, angioma); they are rare and do not have a practical value.
Malignant tumours are divided into primary and secondary, or metastatic. Among malignant tumours often is a cancer.
Lungs cancer
The lungs cancer develops unnoticed, almost nothing can be find out itself, that is why 60-70% patients come to the doctor already with the started forms of disease. By the clinical symptoms of lungs cancer on the first stages of disease are rapid fatigueability, weight loss, pain in breasts, cough, sometimes at cough is a sputum patient notices the veins of blood. At the laboratory analysis of blood promoted ERS is marked, anaemia.
A cancer in lungs is almost always developed from the epithelium of bronches; large bronches often struck: main and lobar, rarer segmentar and yet rarer shallow periferial. From lobar bronches the bronches of superior lobe of right are mostly struck lungs.
From plenty of the offered classifications of this disease the most widespread is the classification of Y.M.Socolov (1956), who distinguishes such forms of lungs cancer:
Primary:
1) Central (endo-, exo-, peribronchial);
2) Peripheral (spherical and cavital);
3) Untypical forms (mediastinal, apex (Penkosta) and miliar carcinosis).
Secondary:
1) Metastases.
A central cancer of lungs develops from the epithelium of main, lobar or segmentar bronches. In one cases a tumour grows mainly in the road clearance of bronchus - endobronchial, in other – exobronchial and peribronchial round a bronchus, germinating in contiguous pulmonary tissue.
The clinical symptoms of central cancer appear in that stage of the development of tumour, when violation of the external respiratory, drainage function of bronchus, inflammatory reaction of adjoining tissues, are present.
The roentgenological pattern of central cancer consists of displays of tumour, signs of violation of bronchus communicating, complications which arise up in connection with progresive growth of tumour and its metastases. The decline of radiolucency of lobe is marked and all the lungs, which increase lung pattern appears on a background, narrowing of intercostal intervasal, something is promoted position of diaphragm cupula and insignificant displacement of mediastinal organs, mainly to the esophagus (at contrasting his examination) and trachea.
At endobronchial cancer tumour of obturate formations (see section 15)of bronchus which brings an origin over of hypoventilation or atelectasis and development of concomitant inflammation. A node of tumour on the first stages of the development can be expressly marked off from adjoining tissue. However, to the extent of progress of tumour process he loses clear scopes and begins to spread outside a bronchus in lungs tissues. Computer and ordinary tomography finds out a tumour, that obturue road clearance of bronchus.


Fig.18.1 Atelectasis of the left lungs as a result of obturation of left main bronchus, bronchogramic obturation of the under lobar bronchus by a cancer tumour (symptom of bronchus amputation).
At the exobronchial type(see fig 18.2) of growth a tumour appears only then, when its sizes more than diameter of large pulmonary vessels. At the beginning the development of the bronchial communicating tumour violations. Only later, during infiltration of wall of bronchus, and then increase of tumour there are too a few centimetres, there are violations of ventilation (hypoventilation, valvular emphysema, and atelectasis). Lungs roots are extended, unstructured, and hard.
Fig.18.2 A central exobronchial cancer of the left lung
At the peribronchial type of growth tumours appear thick muffs round bronches and vessels. The increased lung pattern, which in next grows into rough hard which fan-shaped walk away from a root in pulmonary tissue, is determined. Formations of bronches remain clock-houses, signs of violation of ventilation lungs do not appear. Computer and ordinary tomography finds out the bulge of bronchial walls and visualised tumour mass, bronchographa is the concentric even narrowing of road clearance of bronches on a considerable draught, related to the bulge of their wall.
A peripherial cancer (see fig 18.3) arises out of epithelium of mucus shell of subsegmentar bronches and bronchioles. The clinical symptoms of this form of cancer depend on situating of tumour node in relation to a thoracic wall or large bronches. Growing in of tumour in pleura causes pain in the area of thorax. When a tumour gets to the large bronchus, a cough appears, sputum, hemoptysis.

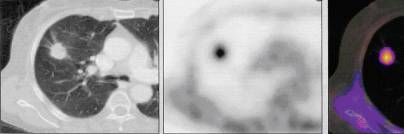
Fig.18.3 The peripheral cancer is on a sciagram, CT PAT.
Roentgenological and CÒ-examination finds out a peripheral cancer as a node a diameter 2-4 sm and anymore, as a rule, in the superior lobes of lungs, more often business. The important signs of peripheral lungs cancer are: 1) wrong spherical form, visualised on CT and roentgenological multiaxial examination of patient; 2) determined on roentgenograms, ordinary and computer tomography heterogeneous structure of tumour shade which consists of separate nodes; 3) unequal, hilly, on separate areas unclear, the contours of shade are smeared; 4) pulmonary tissue is unchanged round shade of cancer node; 5) presence on occasion "paths" to the root lungs, predefined the shallow metastatic pouring out, or germination of tumour along lymphatic vessels (cancer lymphangoitis); 6) regional defects of walls of bronches which are determined on occasion at bronchography; 7) bulge of pleura, joint, accretion, or pleural exudate which are observed at the near placing of pleural tumour; 8) cavity of wrong form with unequal edges, without a horizontal level which appears at disintegration of tumour and appears on a sciagram, CT and ordinary tomogramas

Fig.18.4 a )Cavitar form of cancer

b) mediastinal cancer
The mediastinal cancer (see fig 18.4 b) of lungs is the display of metastatic of primary cancer tumour, which is more often placed at the level of bifurcation of trachea, medial wall of main or lobar bronches. There is metastasing in tracheobronchial and paratracheal lymphatic nodes. Clinically characterized by the reduction syndrome of defeat of mediastinum (syndrome of superior vena cava, reduction of esophagus, turning and diaphragmal nerves), in particular by the edema of fase and neck. A roentgenological pattern characterizes the presence of large shade from one side, which closes shade of root. Hyperplasy of staggered lymphatic nodes appears on CT-skans.
An apex cancer (cancer Penkosta) (see fig 18.5 a) is a cancer of superior lobe lungs. His early germination in ribs and involvements the process of nervous interlacements stipulates a clinical pattern: pain in a humeral joint, thorax, and also Gorner`s syndrome (of superior eyelid, enophtalm, narrowing of pupil). However many symptoms of already started process which spread outside lungs. The roentgenological pattern of apex cancer characterizes homogeneous shade in the area of apex lungs. Characteristic is destruction of back segments of one-two ribs, and also transversal sprouts of a few vertebrae.
à  b
b 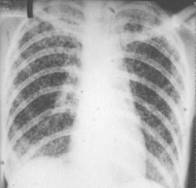
Fig.18.5. Cancer Penkosta (a) miliar carcinosis (b)
Miliar carcinomatous (carcinosis) (see fig 18.5 b) is not indiform of tumour growth, but is only one of the forms of his metastatic - hematogenous skidding of tumour mews. A primary tumour node is small and does not appear during roentgenological and CÒ-examinationes. Plural shades appear on rent-genogramas and computer tomogramas; by a size to 3 mm. Shades increase afterwards, anymore in inferior lobes. A lung pattern is not traced.
Metastatic tumours of lungs
Metastases in lungs (see fig 18.6) can give any primary malignant tumours, present in other organs and tissues of organism. However often they are observed at cancer of suckling gland, stomach, adrenal glands, at an osteogenic sarcoma, chorionepitelioma. The characteristic feature of metastases is their multiplicity.
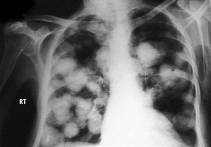
Fig.18.6 Metastases of cancer are in lungs
Lung and pleural traumatic damages (see fig 18.7)
The traumas of thorax are divided into: opened (penetrable) and closed (dull). On a method, causing first divide into gunshat, stab, cut, and second - as a result of blow, falling, clench. Victims grumble about pain in the area of breasts, stuffiness, and hyperhidrosis. The pallor of skin, tachycardia, appears during a review, painless in the damaged place, there can be a hemorrhage and hypodermic emphysema, acute respiratory insufficiency, shock.
Traumas which are accompanied the break of ribs are often complicated as a result of break of pulmonary tissue, visceral pleura and hit of air in a pleura cavity. Air in a pleura cavity can get and from outside through a wound. Roentgenological at pneumothorax the brightening and the lung pattern absence appear in the damaged half of thorax for peripheries.
1  2
2  3
3 
Fig.18.7 pneumothorax (1, 2), hypodermic emphysema (3)
In the case of opened pneumothorax air can spread between soft tissues of the thorax and there is hypodermic emphysema which clinically detection appears by palpation, and roentgenological - by appearance of "feather-like" pattern at the lungs level as the result of muscles stratification of by air.
Often pneumothorax is accompanied by the break of vessels, hemorrhage in a pleura cavity and origin of hemopneumothorax. Roentgenologicaly in the superior departments of the damaged half of thorax brightening appears with absence of the lung pattern, and in homogeneous shade with a gorizontal level which remains such in any position of body.
Spontaneous pneumothorax can be as a result of complications of different lungs diseases (tuberculosis, emphysema, and cyst) from involvement in the pathological process of visceral pleura and its break.
Pneumothorax is better diagnosed by CT, which can find out even the small quantity of air in any pleura recesss (vertebro-mediastinal recess), and also air which got in mediastinum through the torn bronchus and spreads for peribronchial and perivascular spaces.
The bronches and lungs foring bodies
The foreign bodies of bronches and lungs divide by exogenous (the penetrating from an external environment|Wednesday|) and endogenous (from the lungs and mediastinal lymphatic nodes or appearing in lungs and bronches). Distinguish radioapaque| and non-radioapaque | foreign bodies.
Exogenous foring bodies more frequent meet at children|kids| of the first year which aspirated | different|diverse| foreign bodies: needles, pins, paper clips, buttons, parts|portions| of toys, own baby teeth, stone|bones| of different|diverse| garden-stuffs, seed of sunflower, and etc.
In easy|light| foreign bodies get either as a result of wound of thorax or as a result of perforation of bronchus by a foreign body.
Clinical signs are: the sudden persistent cough, attacks of asphyxia and vomiting, cyanosys. After a while the signs of inflammation and suppuration of pulmonary tissue become anchorwomens.
The basic|main| methods of the diagnostics: roentgenologic and bronchoscopy |.
Diagnostics of the radioapaque|| foreign bodies is based on| sciagraphy of lungs in two perpendicular | projections, on roentgenogramas| dense|tight| shade|shadow|, proper to the form|shape|, sizes|dimensions| and position|rule| of foreign body, is revealed. If necessary conduct roentgenoscopy|, tomography| and bronchoscopy|.
Diagnostics of non-radioapaque | foreign bodies is based on determination|definition| of the bronchus ability violation degree with using the functional tests and bronchography|, CT.
The pulmonary edema
It is |surplus accumulation of the liquid part|portion| of blood in alveoles and connecting | tissue, containing|maintaining| squirrel, electrolytes and several cellular elements.
Classification:
I. The non-inflammatory | edemas
1. Stagnant edemas
a) At the circulatory system:
1) acute edema of the lungs;
2) sub-acute and chronic lungs edema;
3) terminal, hypostatic| lungs edema;
á) In the lymphatic system: at thelimphatic system damage|, becous of| tuberculosis, tumours|swelling|.
2. Exchanges edemas: at a cachexy, starvation, violations external and internal incretion, at the blood diseases.
II. The INFLAMMATORY EDEMAS
1. aerogenes: bacterial, aspirational|, toxic (inhalations);
2. hematogenes|;
3. neurogenes|: a|but|) central origin; b) peripheral
The acute (more frequent cardiogenic|) edema (see fig 18.8) develops as a result of increase|rise| of pressure in the small circle of the blood circulation and vasomotour| violations and also increase|rise| of the capillaries walls permeability.
Clinic: difficulty in breathing, sense|feeling,sentiment| of amotivational fear, pallor, sweating|, shallow breathing (35—40 breathings in a minute) painful|agonizing| incessant cough with a foamy sputum, hemoptysis|.
Roentgenologic signs: uneven declineof the|lowering|| lungs sub-roots departments pneumatisation due to appearance of the focal shades|shadows| with different|diverse| sizes|dimensions| inclined to|by| confluence; the lungs roots are extended, unstructural; the lung pattern of both lungs is increased, washed out; the defeat is bilateral|two-way|, anymore shown in a right lung; the sizes|dimensions| of the heart are megascopic. The rapid|quick,fast| dynamics of roentgenologic picture|painting| is|appears| the characteristic|character,typical| sign of the lungs edema under the treatment influencing.
At the chronic lungs edema the defeat of the lungs inferior|bottom| departments and accumulation of the liquid in a pleura are visualised.
The exchanges, toxic and neurogenic| lungs edemas differ from cardiogenic by absence of the cardiac|hearty,kind| shade changes|shadow|.
The typical sign of the interstitial| edema - the presence of linear shades|shadows| ( The Cerly’s lines|).
a  b
b 
Fig.18.8 The surveying|survey| lungs roentrenography: a) pulmonary edema. The foci-like shades are |shadows| sometimes meeting between itself. b)the pulmonary interstitial edema.
Thromboemboly of pulmonary artery
Thromboemboly of pulmonary artery (TEPA)(see fig 18.9) takes place as a result of pulmonary truncus some branches obturation by a blood clot. More frequent all happens as the result of complication in the after-operational period, or the patients in tied down to the bed, when thrombophlebitis of inferior extremities develops. Roentgenological appears darkening with unclear contours, pleura exudate is possible. Obturation of large branches of pulmonary truncus results in an acute pulmonary heart, when the right departments of the heart are increased and superior vena cava and arc of pulmonary truncus broadens. Perfusional scintigraphy at TEPA finds out in lungs an area with reduced perfusion. Angiopulmonography specifies oclusion of what pulmonary artery took a place.
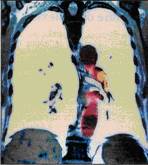
Fig.18.9 Coloured spiral CT thromboemboly of left pulmonary artery branch
The algorithm of the birthing organs radio examination includes|switches| the following methods: fluorography|, sciagraphy, fluoroscopy|, linear tomography|, computer tomography |, magnetically-resonance imaging|, scintigraphy|, SPECÒ|, PAT, radionuclear| scanning, radiometry, and sonography|, which are used in obedience to|in accord with,according to| principle – from more simple to|by| more difficult|complex|:
1)Basic|main|: sciagraphy, fluorography, sciascopy |;
2)Additional:
are methods of the secondary turn: the linear tomography, CÒ|;
3) Special:
are non-invasive and small-invasive|: US, ÌÐI|, scintigraphy |, CT-angiography|, ÌÐ- angiography |;
are invasive|: the bronchography|, angiopulmonography|, the bronchial arteries angiography|.
Date: 2014-12-28; view: 3553
| <== previous page | | | next page ==> |
| Tuberculosis | | | LEGAL FORMS OF ORGANIZATION |