
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
TABLE IV-114 Risk Factors for Active Tuberculosis Among Persons Who Have Been Infected With Tubercle Bacilli 36 page
A. Electroencephalogram (EEG)
B. IV loading with antiepileptic medication
C. Lumbar puncture
D. Magnetic resonance imaging
E. Substance abuse counseling
XI-14. All of the following statements regarding epilepsy are true EXCEPT:
A. The incidence of suicide is higher in epileptic patients than it is in the general population.
B. Mortality is no different in patients with epilepsy than it is in age-matched controls.
C. A majority of patients with epilepsy that is completely controlled with medication eventually
will be able to discontinue therapy and remain seizure-free.
D. Surgery for mesial temporal lobe epilepsy (MTLE) decreases the number of seizures in over
70% of patients.
E. Tricyclic antidepressants lower the seizure threshold and may precipitate seizures.
XI-15. A 20-year-old woman is brought to the emergency department after a witnessed generalized tonic-clonic seizure. She has no identifying information, and her past medical history is unknown. What is the most likely cause of her seizure?
A. Amyloid angiopathy
B. Fever
C. Genetic disorder
D. Illicit drug use
E. Uremia
XI-16. A 36-year-old man is brought to the emergency department because of a seizure. His family reports he has a history of seizure disorder but stopped his medications a month ago due to financial issues. He had a brief seizure at home that stopped within a few minutes. However, 15 minutes later he began seizing again and the tonic-clonic activity has persisted for 30 minutes. On physical examination he is afebrile, hypertensive, and actively seizing. All of the following are potential therapies for his condition EXCEPT:
A. Carbamazepine
B. Fosphenytoin
C. Lorazepam
D. Phenobarbital
E. Valproate
XI-17. The most common cause of a cerebral embolism is:
A. Atrial fibrillation
B. Cardiac prosthetic valves
C. Dilated cardiomyopathy
D. Endocarditis
E. Rheumatic heart disease
XI-18. A 54-year-old male is referred to your clinic for evaluation of atrial fibrillation. He first noted the irregular heartbeat 2 weeks ago and presented to his primary care physician. He denies chest pain, shortness of breath, nausea, or gastrointestinal symptoms. Past medical history is unremarkable. There is no history of hypertension, diabetes, or tobacco use. His medications include metoprolol. The examination is notable for a blood pressure of 126/74 mmHg and a pulse of 64 beats/min. The jugular venous pressure is not elevated. His heart is irregularly irregular, with normal S1 and S2. The lungs are
clear, and there is no peripheral edema. An echocardiogram shows a left atrial size of 3.6 cm. Left ventricular ejection fraction is 60%. There are no valvular or structural abnormalities. Which of the following statements regarding his atrial fibrillation and stroke risk is true?
A. He requires no antiplatelet therapy or anticoagulation because the risk of embolism is low.
B. Lifetime vitamin K antagonist therapy is indicated for atrial fibrillation in this situation to reduce
the risk of stroke.
C. He should be admitted to the hospital for IV heparin and undergo electrical cardioversion;
afterward there is no need for anticoagulation.
D. His risk of an embolic stroke is less than 1%, and he should take a daily aspirin.
E. He should be started on SC low-molecular-weight heparin and transitioned to warfarin.
XI-19. All the following have been shown to reduce the risk of atherothrombotic stroke in primary or secondary prevention EXCEPT:
A. Aspirin
B. Blood pressure control
C. Clopidogrel
D. Statin therapy
E. Warfarin
XI-20. A 57-year-old man is brought to the emergency department after falling while playing tennis and developing garbled speech. He has a past history of hypertension and hypercholesterolemia. His medications include atorvastatin and enalapril. On physical examination, his blood pressure is 210/115 mmHg with heart rate 105 beats/min, respirations 28 breaths/min, temperature 37°C (98.6°F), and oxygen saturation 94% on room air. He is alert but aphasic with upper and lower left extremity
hemiparesis. He is able to move his right side normally. Based on the results of immediate imaging, all of the following are potential therapeutic considerations for his condition EXCEPT:
A. Anticoagulation
B. Blood pressure lowering
C. Hypothermia protocol
D. Intracerebral stent placement
E. IV thrombolysis
XI-21. Which of the following statements regarding Alzheimer’s disease is true?
A. Delusions are uncommon.
B. It accounts for over half of the cases of significant memory loss in patients over 70 years of age.
C. It typically presents with rapid (<6 months) significant memory loss.
D. Less than 5% of patients present with nonmemory complaints.
E. Pathologically, the most notable abnormalities are in the cerebellar regions.
XI-22. All of the following medications have been shown to have potential efficacy in the treatment of Alzheimer’s disease EXCEPT:
A. Donepezil
B. Galantamine
C. Memantine
D. Oxybutynin
E. Rivastigmine
XI-23. A 72-year-old right-handed male with a history of atrial fibrillation and chronic alcoholism is evaluated for dementia. His son gives a history of a stepwise decline in the patient’s function over the last 5 years with the accumulation of mild focal neurologic deficits. On examination he is found to have a pseudobulbar affect, mildly increased muscle tone, and brisk deep-tendon reflexes in the right upper extremity and an extensor plantar response on the left. The history and examination are most consistent with which of the following?
A. Alzheimer’s disease
B. Binswanger’s disease
C. Creutzfeldt-Jakob disease
D. Multi-infarct dementia
E. Vitamin B12 deficiency
XI-24. A 49-year-old woman presents for a second opinion regarding symptoms of tremors, difficulty with ambulation, and periodic flushing. Her symptoms originally began approximately 3 years ago. At that time, she was hospitalized for a syncopal episode, after which she was told to increase her salt intake. Since then, she has had progressive motor difficulties including bilateral tremors and a stiff, slow gait. She also has had several more episodes of syncope. She states that she knows when these syncopal events will occur because she feels faint and weak. She has never had an injury from syncope. A final recent symptom has been periodic flushing and sweating. A neurologist previously diagnosed
her with Parkinson’s disease and prescribed therapy with ropinirole. Despite increasing doses, she does not feel improved, but rather has recently noticed uncontrollable movements that she describes as tics of her face. Her only other medical history is recent recurrent urinary tract infections. Her medications are ropinirole 24 mg daily and nitrofurantoin 100 mg daily. She reports no history of drug use. On physical examination, her blood pressure is 130/70 mmHg with a heart rate of 78 beats/min while sitting. Upon standing, her blood pressure drops to 90/50 mmHg with a heart rate of 110 beats/min. Her ocular movements are full and intact. She has recurrent motor movements of the right side of her face. Her neurologic examination shows increased muscle tone in the lower extremities with bilateral 4-Hz tremor. Deep tendon reflexes are brisk and 3+ in upper and lower extremities. Three beats of myoclonus are present at the ankles bilaterally. She walks with a spastic gait. Strength is normal. What is the most likely diagnosis?
A. Corticobasal degeneration
B. Diffuse Lewy body dementia
C. Drug-induced Parkinson’s disease
D. Multiple system atrophy with parkinsonian features
E. Parkinson’s disease with inadequate treatment
XI-25. A 65-year-old man presents to your office complaining of a tremor and progressive gait abnormalities. He states that he first noticed a slowing of his gait approximately 6 months ago. He has difficulty rising to a standing position and states that he shuffles when he walks. In addition, he states that his right hand shakes more so than his left, and he is right handed. He believes it to be worse when not moving but states there are times when he spills his morning coffee because of the tremors. He has retired but states he is not able to play tennis and golf any longer because of his motor symptoms. He denies syncope or presyncope, difficulty swallowing, changes to his voice, or memory difficulties. His past medical history is significant for hypertension and hypercholesterolemia. His medications are hydrochlorothiazide 25 mg daily, ezetimibe 10 mg daily, and lovastatin 40 mg daily. He drinks a glass of wine with dinner daily and is a lifelong nonsmoker. On physical examination, he has masked facies. His gait shows decreased arm swing with slow shuffling steps. He turns en bloc. A pill-rolling tremor is present on the right side. There is cogwheel rigidity bilaterally. Eye movements are full and intact. There is no ortho-static hypotension. A brain MRI with gadolinium shows no evidence of mass lesions, hydrocephalus, or vascular disease. You diagnose the patient with Parkinson’s disease. The patient asks about his prognosis and likelihood of disability. Which of the following is correct about the clinical course and treatment of Parkinson’s disease?
A. Early initiation of therapy with levodopa predisposes an individual to a higher likelihood of
dyskinesias early in the disease.
B. Early therapy with bilateral deep-brain stimulation of the subthalamic nuclei slows the
progression of Parkinson’s disease.
C. Initial treatment with a dopamine agonist such as pramipexole is likely to be effective in
controlling his motor symptoms for 1–3 years before the addition of levodopa or another agent is
necessary.
D. Levodopa should be started immediately to prevent the development of disabling rigidity.
E. MAO inhibitors are contraindicated once the diagnosis of Parkinson’s disease is established.
XI-26. All of the following statements regarding restless legs syndrome (RLS) are true EXCEPT:
A. Dopamine antagonists are effective therapy.
B. Most patients develop symptoms before the age of 30 years old.
C. RLS may cause sleep disorder and daytime hyper-somnolence.
D. RLS is more common in Asians than in the general U.S. population.
E. Symptoms may involve the upper extremity.
XI-27. A 63-year-old man seeks medical attention because of progressive weakness of the left foot and lower leg over the last 6 months. The progression has been gradual, and he only noticed it initially because of cramping and tripping while playing squash. He denies back pain. His only medication is atorvastatin. On physical examination, vital signs are normal and the only abnormalities are on neurologic examination. His left leg strength is notably diminished in the hip flexors, hip adductors, quadriceps, and calf muscles. There is atrophy of the quadriceps and calf. His ankle and knee reflexes are increased on the left. He has subtle weakness on the right quadriceps. There are no sensory abnormalities in light touch, pinprick, temperature, or proprioception. There are occasional fasciculations of the abdominal muscles. Before diagnosing the patient with amyotrophic lateral sclerosis (ALS), all of the following alternative diagnoses should be ruled out EXCEPT:
A. Cervical spondylosis
B. Foramen magnum tumor
C. Lead poisoning
D. Multifocal motor neuropathy with conduction block
E. Vitamin C deficiency
XI-28. A 42-year-old woman seeks medical attention for a 5- to 6-week history of marked fatigue that is affecting her work. She reports that she has felt some general fatigue but her symptoms are most notable when she starts moving around during the day. She has taken her pulse and it feels fast to her. She reports no loss of consciousness, but does say that she feels lightheaded and has blurred vision after arising. Sitting or lying down improves the symptoms. She has no notable past medical history and takes no medications other than a calcium/vitamin supplement. On physical examination, her supine heart rate is 90 beats/min with blood pressure of 110/70 mmHg. Upon standing her heart rate increases to 130 beats/min and is regular, and her blood pressure standing is 115/75 mmHg. She reports lightheadedness during the episode. An ECG while symptomatic shows sinus tachycardia without any conduction abnormalities. Which of the following is the most likely diagnosis?
A. Addison’s disease
B. Autoimmune autonomic neuropathy
C. Diabetic neuropathy
D. Multisystem atrophy
E. Postural orthostatic tachycardia syndrome
XI-29. A 45-year-old male complains of severe right arm pain. He gives a history of having slipped on the ice and severely contusing his right shoulder approximately 6 months ago. Soon thereafter, he developed sharp, knifelike pain in the right arm and forearm that lasted for a few months. There was some arm swelling and warmth. He was evaluated in an urgent care setting. There were no radiographic abnormalities and he was not treated. Since the injury, the pain and swelling have persisted. Physical
examination reveals a right arm that is more moist and hairy than the left arm. There is no specific weakness or sensory change. However, the right arm is clearly more edematous than the left, and the skin appears shiny and cool. The patient’s pain most likely is due to:
A. Acromioclavicular separation
B. Brachial plexus injury
C. Cervical radiculopathy
D. Complex regional pain syndrome
E. Subclavian vein thrombosis
XI-30. Which of the following criteria suggests the diagnosis of trigeminal neuralgia?
A. Deep-seated, steady facial pain
B. Elevated erythrocyte sedimentation rate (ESR)
C. Objective signs of sensory loss on physical examination
D. Response to gabapentin therapy
E. None of the above
XI-31. A 72-year-old woman presents with recurrent episodes of incapacitating facial pain lasting from second to minutes and then dissipating. The episodes occur usually twice per day, usually without warning, but are also occasionally provoked by brushing of her teeth. On physical examination, she appears well with normal vital signs. Detailed cranial nerve examination reveals no sensory or motor abnormalities. The remainder of her neurologic examination is normal. What is the next step in her management?
A. Brain MRI
B. Brain MRI plus carbamazepine therapy
C. Carbamazepine therapy
D. Glucocorticoid therapy
E. Referral to Otolaryngology for surgical cure
XI-32. A 72-year-old female presents with brief, intermittent excruciating episodes of lancinating pain in the lips, gums, and cheek. Touching the lips or moving the tongue can initiate these intense spasms of pain. The results of a physical examination are normal. MRI of the head is also normal. The most likely cause of this patient’s pain is:
A. Acoustic neuroma
B. Amyotrophic lateral sclerosis
C. Meningioma
D. Trigeminal neuralgia
E. Facial nerve palsy
XI-33. A 33-year-old woman presents with rapidly worsening pain at the top of the back over the last 3 days. The pain is not relieved by lying down or by wearing a soft neck collar. She notes that the pain is much worse with movement and has woken her from sleep. The pain is severe and is impeding her daily activities. She denies any arm pain or weakness. There is no history of prior back or neck pain,
trauma, or arthritis. She works as a postal delivery agent and her only physical activity is walking. She is monogamous with her husband and has no illicit activities. Her family history is notable for an aunt and mother with breast cancer. Her MRI is shown in Figure XI-33. Which is the most likely diagnosis?

FIGURE XI-33
A. Cervical spondylosis
B. Hematomyelia
C. Metastatic breast cancer
D. Spinal epidural abscess
E. Spinal epidural hematoma
XI-34. A 34-year-old female complains of lower extremity weakness for the last 3 days. She has noted progressive weakness in the lower extremities with loss of sensation “below the belly button” and incontinence. She had had some low-grade fevers for the last week. She denies recent travel. Past medical history is unremarkable. Physical examination is notable for a sensory level at the level of the umbilicus. The lower extremities show +3/5 strength bilaterally proximally and distally. Reflexes, cerebellar examination, and mental status are normal. All of the following are appropriate steps in evaluating this patient EXCEPT:
A. Antinuclear antibodies
B. Electromyography
C. Lumbar puncture
D. MRI of the spine
E. Viral serologies
XI-35. Which of the following statements about syringomyelia is true?
A. More than half the cases are associated with Chiari malformations.
B. Symptoms typically begin in middle age.
C. Vibration and position sensation are usually diminished.
D. Syrinx cavities are always congenital.
E. Neurosurgical decompression is usually effective in relieving the symptoms.
XI-36. A 17-year-old adolescent is seen in the clinic several weeks after he suffered a concussion during a high-school football game. At the time of the event, paramedics reported that he experienced no loss of consciousness but was confused for a period of about 10 minutes. Head imaging was normal. He describes a generalized headache that is present all the time since his trauma, and he occasionally feels dizzy. His mother is concerned that he is having a hard time concentrating in school and seems depressed to her lately; she describes him as being very energetic prior to his concussion. The patient’s physical examination is entirely normal except for a somewhat flattened affect. Which of the following statements regarding his condition is true?
A. He has an excellent prognosis.
B. He meets the criteria for postconcussive syndrome and should improve over 1–2 months.
C. He should avoid contact sports for 2 weeks.
D. He is most likely malingering.
E. Low-dose narcotics should be started for headache.
XI-37. A 68-year-old man is brought to the clinic by his wife for evaluation. She has noticed that over past 2–3 months her husband has had increasingly slowed thinking and a change in his personality in that he has become very withdrawn. His only complaint is a mild but persistent, diffuse headache. There is no history of head trauma, prior neurologic or psychiatric disease, or family history of dementia. Physical examination is only notable for a moderate cognitive deficit with a mini-mental examination of 19/30. His head CT is shown in Figure XI-37. What is the most likely diagnosis?
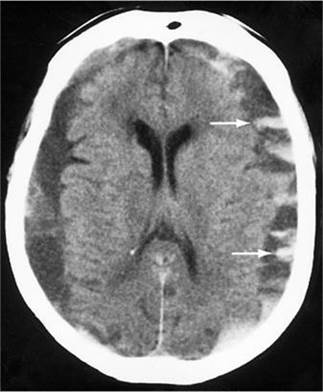
FIGURE XI-37
A. Acute epidural hematoma
B. Acute subarachnoid hemorrhage
C. Alzheimer’s disease
D. Chronic subdural hematomas
E. Normal-pressure hydrocephalus
XI-38. A 76-year-old nursing home resident is brought to the local emergency department after falling out of bed. The fall was not witnessed; however, she was suspected to have hit her head. She is not responsive to verbal or light tactile stimuli. At baseline she is able to converse but is frequently disoriented to place and time. She has a medical history that includes stable coronary disease, mild emphysema, and multi-infarct dementia. Immediately after triage she is taken for a CT scan of the head. Which of the following is true regarding head injury and hematomas?
A. More than 80% of patients with subdural hematomas will experience a lucid interval prior to
loss of consciousness.
B. Epidural hematomas generally arise from venous sources.
C. Epidural hematomas are common among the elderly with minor head trauma.
D. Most patients presenting with epidural hematomas are unconscious.
E. Subdural hematomas lead to rapid increases in intracranial pressure and can require arterial
ligation.
XI-39. A 49-year-old man is admitted to the hospital with a seizure. He does not have a history of seizures and he currently takes no medications. He has AIDS and is not under any care at this time. His physical examination is most notable for small, shoddy lymphadenopathy in the cervical region. A head CT shows a ring-enhancing lesion in the right temporal lobe, with edema but no mass effect. A lumbar puncture shows no white or red blood cells, and the Gram stain is negative. His serum Toxoplasma IgG is positive. He is treated with pyrimethamine, sulfadiazine, and levetiracetam. After 2 weeks of therapy the central nervous system (CNS) lesion has not changed in size and he has not had any more seizures. All microbiologic cultures and viral studies, including Epstein-Barr virus DNA from the cerebrospinal fluid, are negative. What is the best course of action for this patient at this time?
A. Continue treatment for CNS toxoplasmosis.
B. Dexamethasone.
C. IV acyclovir.
D. Stereotactic brain biopsy.
E. Whole-brain radiation therapy.
XI-40. A young man with a history of a low-grade astrocytoma comes into your office complaining of weight gain and low energy. He is status post resection of his low-grade astrocytoma and had a course of whole-brain radiation therapy (WBRT) 1 year ago. A laboratory workup reveals a decreased morning cortisol level of 1.9 μg/dL. In addition to depressed adrenocorticotropic hormone (ACTH) function, which of the following hormones is most sensitive to damage from whole-brain radiation therapy?
A. Growth hormone
B. Follicle-stimulating hormone
C. Prolactin
D. Thyroid-stimulating hormone
XI-41. A 37-year-old woman with a history of 6 months of worsening headache is admitted to the hospital after a tonic-clonic seizure that occurred at work. The seizure lasted a short time and terminated spontaneously. On examination her vital signs are normal, she is somnolent but awake, and there are no focal abnormalities. Her initial CT scan showed no acute hemorrhage but was abnormal. An MRI is obtained and is shown in Figure XI-41. What is the most likely diagnosis in this patient?
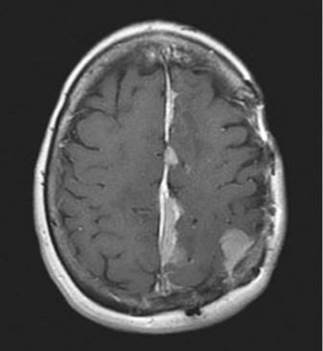
FIGURE XI-41
A. Brain abscess
B. Glioblastoma
C. Low-grade astrocytoma
D. Meningioma
E. Oligodendroglioma
XI-42. All of the following are frequent initial symptoms of multiple sclerosis EXCEPT:
A. Optic neuritis
B. Paresthesias
C. Sensory loss
D. Visual loss
E. Weakness
XI-43. Which of the following is the most common clinical classification of multiple sclerosis?
A. Autoimmune autonomic neuropathy
B. Primary progressive
C. Progressive relapsing
D. Relapsing/remitting
E. Secondary progressive
XI-44. Lumbar puncture should be preceded by CT or MRI in all of the following subsets of patients suspected of having meningitis EXCEPT those with:
A. Depressed consciousness
B. Focal neurologic abnormality
C. Known central nervous system (CNS) mass lesion
D. Positive Kernig’s sign
E. Recent head trauma
XI-45. A 78-year-old man with diabetes mellitus presents with fever, headache, and altered sensorium. On physical exam his temperature is 40.2°C (104.4°F), heart rate is 103 beats/min, and blood pressure is 84/52 mmHg. His neck is stiff and he has photophobia. His cerebrospinal fluid (CSF) examination shows 2100 cells/μL, with 100% neutrophils, glucose 10 mg/dL, and protein 78 mg/dL. CSF Gram stain is negative. In addition to empiric antibacterial antibiotics, initial therapy should include which of the following?
A. Acyclovir
B. Dexamethasone after antibiotics
C. Dexamethasone prior to antibiotics
D. IV γ globulin
E. Valacyclovir
XI-46. Which of the following groups of patients should receive empirical antibiotic therapy that includes coverage of Listeria monocytogenes in cases of presumed meningitis?
A. Immunocompromised patients
B. Elderly patients
C. Infants
D. All of the above
XI-47. Which of the following medicines has been most commonly implicated in the development of noninfectious chronic meningitis?
A. Acetaminophen
B. Acyclovir
C. β-lactam antibiotics
D. Ibuprofen
E. Phenobarbital
XI-48. Variant Creutzfeldt-Jakob disease (vCJD) has been diagnosed in which of the following populations?
A. Family members with well-defined germ-line mutations leading to autosomal dominant
inheritance of a fatal neurodegenerative disease
B. New Guinea natives practicing cannibalism
C. Patients accidentally inoculated with infected material during surgical procedures
D. Worldwide, in sporadic cases, mostly during the fifth and sixth decades of life
E. Young adults in Europe thought to have been exposed to tainted beef products
XI-49. The presence of startle myoclonus in a 60-year-old man with rapidly progressive deficits in cortical dysfunction is which of the following?
A. Neither sensitive nor specific for Creutzfeldt-Jacob disease (CJD) but does represent grounds to
explore further for this condition with an electroencephalogram (EEG)
B. Neither sensitive nor specific for CJD but does represent grounds to explore further for this
condition with an EEG and brain MRI
C. Sensitive but not specific for CJD and is not enough to prompt a further workup for this
condition unless other clinical criteria are met
D. Specific but not sensitive for CJD and should therefore prompt immediate referral for brain
biopsy to confirm the diagnosis
E. Virtually diagnostic for CJD, and further workup including EEG, brain MRI, and perhaps brain
biopsy serves only a prognostic purpose
XI-50. A 24-year-old man presents for evaluation of foot-drop. He has noted that for the last several months, he has had difficulty picking his feet up to walk up stairs and over thresholds. His right leg is more affected than his left leg. He has not noted any sensory changes. He has several family members with similar complaints. His exam is notable for distal leg weakness with reduced sensation to light touch in both lower extremities. Knee and ankle jerk reflexes are unobtainable. Calves are reduced in size bilaterally. Upper extremity examination is normal. Which of the following is the most likely diagnosis?
A. Charcot-Marie-Tooth syndrome
B. Fabry disease
C. Guillain-Barré syndrome
D. Hereditary neuralgic amyotrophy
E. Hereditary sensory and autonomic neuropathy
XI-51. A 57-year-old immigrant from Vietnam is evaluated by his primary caregiver for dysesthesias that have been present in his hands and feet for the past several weeks. He also reports some difficulty walking. His past medical history is notable for hypertriglyceridemia, tobacco abuse, and a recently discovered positive PPD with sputum that is smear-negative for Mycobacterium tuberculosis. His medications include niacin, aspirin, and isoniazid. Which of the following is likely to reverse his symptoms?
A. Cobalamin
B. Levothyroxine
C. Neurontin
D. Pregabalin
E. Pyridoxine
XI-52. A 52-year-old woman with long-standing, poorly controlled type 2 diabetes mellitus is evaluated for a sensation of numbness in her fingers and toes, as if she is wearing gloves and socks all the time. She also reports tingling and burning in the same location, but no weakness. Her symptoms have been intermittently present for the last several months. After a thorough evaluation, nerve biopsy is obtained and demonstrates axonal degeneration, endothelial hyperplasia, and perivascular inflammation. Which of the following statements regarding this condition is true?
A. Autonomic neuropathy is rarely seen in combination with sensory neuropathy.
B. The presence of retinopathy or nephropathy does not portend increased risk for diabetic
neuropathy.
C. This is the most common cause of peripheral neuropathy in developed countries.
D. Tight glucose control from now on will reverse her neuropathy.
E. None of the above is true.
XI-53. All the following cause primarily a sensory neuropathy EXCEPT:
Date: 2016-04-22; view: 839