CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Changes in pathology
If there is accidental damage of small blood vessels bleeding stops after a while. This is due to the formation of thrombus or a blood clot in the site of the vessel injury. This process is called blood coagulation, or hemostasis. Currently, there is the classical enzymatic theory of blood clotting – the theory of Schmidt – Moravits. The principles of this theory are presented in the diagram (Fig. 11):
Fig. 11. The scheme of blood coagulation
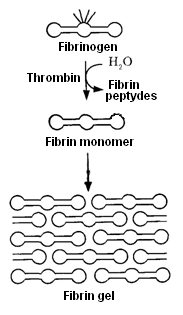
Damage of the blood vessel causes a cascade of molecular processes; as a result the blood clot, or thrombus is formed, stopping leakage of blood. At the site of injury platelets are attached to the opening intercellular matrix; platelet plug is formed. Simultaneously, the system of reactions is activated leading to the conversion of soluble plasma protein fibrinogen into insoluble fibrin, which is deposited in the platelet plug, and on its surface, and the formation of thrombus occurs. The process of blood clotting occurs in two phases. In the first phase prothrombin turns into the active enzyme thrombin under the influence of calcium ions and thrombokinase contained in platelets and liberated from them during the destruction of platelet. In the second phase fibrinogen is converted to fibrin under the influence of the formed thrombin. The whole process of blood coagulation has the following phases of hemostasis: a) the constriction of the damaged vessel; b) the formation at the site of damage loose platelet plug, or white thrombus. Collagen of the vessel serves as a binding agent for platelets. When there is platelet aggregation vasoactive amines are released that stimulate vasoconstriction; c) the formation of red thrombus (blood clot); d) partial or complete dissolution of the clot. White thrombus is formed from blood platelets and fibrin; there are relatively few red blood cells (at a high rate of blood flow). Red thrombus consists of fibrin and red blood cells (in areas of slow blood flow). In the process of blood clotting blood coagulation factors are involved. Clotting factors associated with platelets, are denoted by Arabic numerals (1, 2, 3, etc.), and clotting factors found in blood plasma, are represented by Roman numerals. Factor I (fibrinogen) is glycoprotein. It is synthesized in the liver. Factor II (prothrombin) is glycoprotein. It is synthesized in the liver with the participation of vitamin K. It is able to bind calcium ions. In the hydrolytic cleavage of prothrombin active enzyme of blood clotting is formed. Factor III (tissue factor, or tissue thromboplastin) is formed by tissue damage. It is lipoprotein. Factor IV (Ca2 + ions) is necessary for the formation of active factor X and active tissue thromboplastin, activation of proconvertin, thrombin generation, platelet membranes labilization. Factor V (proaccelerin) is globulin. It is the predecessor of accelerin, is synthesized in the liver. Factor VII (prothrombinogen, proconvertin) – the predecessor of convertin. It is synthesized in the liver, with the participation of vitamin K. Factor VIII (antihemophylic globulin A) is necessary for the formation of active factor X. Congenital lack of factor VIII is the cause of hemophilia A. Factor IX (antihemophylic globulin B, Christmas factor) is involved in the formation of active factor X. When factor IX is in deficiency hemophilia B is developed. Factor X (Staurt - Prower factor) is globulin. X factor is involved in the formation of thrombin from prothrombin. It is synthesized by the liver cells with the participation of vitamin K. Factor XI (Rosenthal factor, plasma thromboplastin antecedent) is antihemophylic factor of protein nature. Failure is observed in hemophilia C. Factor XII (Hageman factor) is involved in the starting mechanism of blood clotting. It stimulates the fibrinolytic activity and other protective reactions of the body. Factor XIII (fibrin-stabilizing factor) is involved in the formation of intermolecular bonds in the fibrin polymer. Factors of platelets. Currently about 10 separate factors of platelets are known. For example: Factor 1 is proaccelerin which is adsorbed on the surface of platelets. Factor 4 is antiheparin factor. Under normal conditions, there is not thrombin in the blood, it is formed from the plasma protein prothrombin by the action of the proteolytic enzyme factor Xa (the index a denotes an active form), which is formed by loss of blood from factor X. Factor Xa converts prothrombin to thrombin only in the presence of Ca2 + and other clotting factors. Factor III, passes into the blood plasma by tissue damage, and platelet factor 3 sets the precondition for the formation of the primer amount of thrombin from prothrombin. It catalyzes the conversion of prothrombin and proconvertin into accelerin (factor Va) and convertin (factor VIIa). During the interaction of these factors, as well as Ca2 + ions factor Xa is formed. Then there is the formation of thrombin from prothrombin. Under the influence of thrombin two A peptides and two B peptides are cleaved from fibrinogen. Fibrinogen is converted into soluble fibrin monomer, which polymerizes rapidly to insoluble fibrin polymer, with the participation of fibrin-stabilizing factor – factor XIII (transglutaminase enzyme) in the presence of Ca2+ ions (Fig. 12).
Fig. 12. The formation of fibrin gel
Fibrin clot attached to the matrix in the site of the vessel damage with the participation of the protein fibronectin. Following the formation of fibrin fibers is their contraction, for which energy of ATP and platelet factor 8 (thrombosthenin) is required. In people with hereditary defects of transglutaminase the blood clots as well as in healthy ones, but thrombus is fragile, that’s why secondary bleeding is possible. Bleeding from the capillaries and small vessels has stopped during the formation of thrombocyte cork. To stop bleeding from larger vessels the rapid formation of a firm blood clot is necessary, to minimize blood loss. This is achieved by a cascade of enzymatic reactions with the mechanisms of amplification on many levels.
There are three mechanisms of enzyme activation cascade: 1. Partial proteolysis. 2. Interaction with proteins-activators. 3. Interaction with cell membranes. Enzymes of a procoagulant path contain γ-carboxyglutamic acid. Radicals of carboxyglutamic acid form binding sites of Ca2 +. There isn’t blood coagulation in the absence of Ca2+.
Date: 2016-04-22; view: 941
|