CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
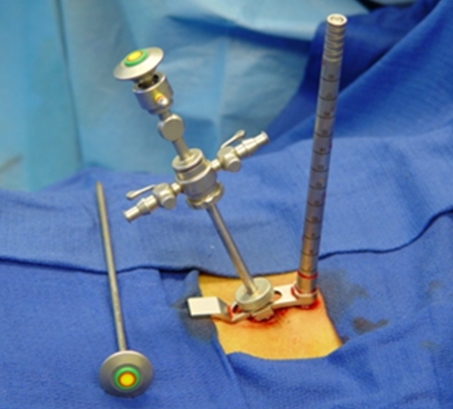
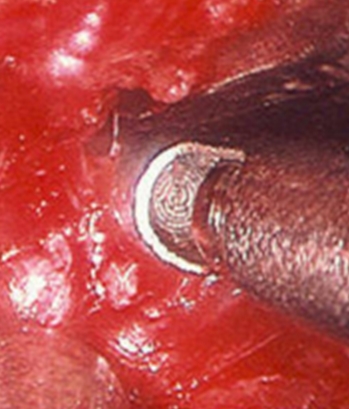
Inserting the EndoscopeAfter visual confirmation is obtained through the access cannula, the dilator is reinserted into the cannula. An arthroscopic sheath with an obturator (sharp or blunt) is inserted through a screw opening on the attached side arm of the working cannula (Figs. 7a & 7b). The SMART® cannula set is designed to allow proper triangulation of the sheath to the cannula endoscopic portal on the distal end of the cannula. The sheath and obturator are advanced until the obturator touches the dilator. At this point, the dilator is removed from the cannula and the sheath gently advanced to just inside the access cannula. The side arm screw is tightened to hold the arthroscope sheath, the obturator is removed, and the endoscope is inserted and locked in place by the bayonet locking mechanism (Figs. 8a–8c). The video camera is then attached to the endoscope to bring the image onto the viewing monitor. 22 Figure 7a: Introduction of endoscopic sheath and obturator Figure 7b: Illustration of introduction of endoscopic sheath and obturator Figure 8a: Endoscope in place for operation Figure 8b: Endoscope in place for operation Figure 8c:Illustration of endoscope in place for operation The endoscope can be used as a primary or auxiliary imaging device, providing improved illumination and magnification of the operative site. It provides visibility and reduces the danger of damage to neural structures during the endoscopically assisted lumbar spine surgery. Fluoroscopy is used to confirm the position of the SMART® tubular retractor (Fig. 9). Figure 9: Fluoroscopic x-ray images of SMART system in surgery - rongeur for laminotomy, discectome in disc space, and curette in action When the tubular retractor is in place, the surgeon can also use alternate methods of visualization, switching between endoscopic and direct viewing, microscopic and endoscopic viewing, or endoscopic viewing alone to accomplish the lumbar microdecompressive surgery. As the surgeon becomes accustomed to the endoscopic view, the microscope may be abandoned, allowing better and wider endoscopic visualization of the entire operative site. Partial caudal laminotomy and medial portion articular process can be resected with a Kerrison bone punch, the curette, or a rasp (Figs. 10a–10d). The ligamentum flavum is then removed (Figs. 11a & 11b) with a rongeur or by incision to expose the lateral lumbar gutter, dural sheath, and lumbar nerve root (Fig. 12). This bony resection facilitates access to the herniated lumbar disc without excessive retraction of the nerve root. Figure 10a: Endoscopic view of the image of the rongeur performing caudal laminotomy for superior lamina Figure 10b: Curetting hypertrophic facet joint Figure 10c: Curetting lumbar lamina Figure 10d: Decompression of the inferior surface of lamina with a rasp Figure 11a: Illustration of Incision and resection of ligamentum flavum Figure 11b: Endoscopic view of Incision and resection of ligamentum flavum Figure 12: Endoscopic view of dissection of nerve root and dura along lateral lumbar gutter After dissection and retraction of the nerve root with the nerve root retractor, the protruded disc is identified and microdecompressive discectomy is performed (Figs. 13a–13c). The SMART® instruments are removed gradually. If necessary, hemostasis can be accomplished with bipolar coagulation. The lumbar fascia and skin edges are closed with simple sutures. Figure 13a: A very large extruded and herniated lumbar disc Figure 13b: Endoscopic view of the large extruded herniated lumbar disc Figure 13c: Removal of a large extruded lumbar disc Often the SMART® Endoscopic Spine System can also be used effectively for decompression of lumbar spinal stenosis and the removal of intraspinal lesions, e.g., synovial cysts (Figs. 14a–14c), large sequestrated lumbar disc fragments, and tumors in the spinal canal. Figure 14a: Large lumbar juxtafacet synovial cyst, at L4-L5 sagital view MRI Figure 14b: Large lumbar juxtafacet synovial cyst, at L4-L5 axial view MRI Figure 14c:Endoscopic view of the residual cyst (short arrow) of a large synovial cyst excised along the lumbar gutter and the dural sac (long arrow) Postoperative Care Post surgically, ambulation begins immediately after recovery and the patient is usually discharged 1 hour after the procedure. They may shower and drive a car the following day. Applying an ice pack is helpful. Nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed as well as mild analgesics and muscle relaxants as needed. The patient can return to usual activities in 10 days to 2 weeks, provided heavy labor and prolonged sitting are not involved. A mild progressive exercise program can begin the day after the surgery. Discussion Obviously, the SMART® Endoscopic Spine System for lumbar spine surgery provides an effective bridge between traditional spine surgery and endoscopic spinal surgery. 21 , 22 The SMART® endoscopic lumbar spine surgery is an effective, safe, less traumatic, and easier form of spine surgery that offers treatment options for nerve decompression, including bulging or herniated discs, bone spurs, degenerative spinal disease, spondylosis, and spinal stenosis. In addition, this technique preserves spinal segmental motion and provides excellent access for spinal arthroplasty. 7 , 21 , 22 This SMART® endoscopic tubular access system offers a number of advantages over existing MISS access approaches. The SMART® system can be used in a dry or fluid medium, can use various imaging combinations, and allows both local anesthesia with conscious sedation, and general anesthesia applications. Most often, the SMART® cannulae allows triangulation of the endoscope micro spinal instruments in the operative field for better visualization which eliminates the bulky holding arms and allows some lateral movement of the cannula within the surgical field. The SMART® tubular access set increases the options available to a spine surgeon, providing true MISS procedures. 22 Conclusions The SMART® Endolumbar Spine System with various sizes of tubular access or trocars (working channels) provides a generous and optimal access for endoscopic MISS of microdecompression of herniated lumbar discs, degenerative spinal disease, spinal stenosis, and removal of intraspinal lesions as well as creating an access for spinal arthroplasty and spinal fixation. With the unique features of the SMART® system, the surgeon can take advantage of microscopic, endoscopic, or direct vision for microdecompressive spinal surgery. This system bridges endoscopic and conventional spinal surgery. This less traumatic, easier, safe and efficacious outpatient MISS treatment leads to excellent results, speedier recovery, and significant economic savings. Date: 2016-03-03; view: 1424
|