CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
Conditions Associated with Acute Leg Ischemia
Chronic Ischemia of the Lower Extremity
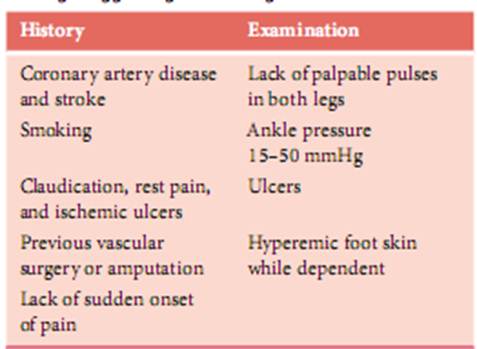
It is sometimes difficult to differentiate between acute leg ischemia, deterioration of chronic leg ischemia, and just severe end-stage chronic disease in general. Periods of pain escalation bring patients with chronic ischemia to the emergency department. Accentuated pain in these patients has a wide range of origins. Decreased foot perfusion can be due to dehydration or lowered systemic pressure as a consequence of heart failure or a change in medication. Ulcers are frequently painful, especially when complicated by infection or when dressings are changed. History and examination of vital functions and the leg usually disclose such conditions and can also sufficiently rule out acute leg ischemia that needs urgent treatment. Patients with chronic ischemia benefit from careful planning of their treatment and should not – with few exceptions – be expeditiously treated. Elective therapy includes weighing risk factors against the outcome of the proposed treatment and all the work-up that is needed to get this information. (It is beyond this book’s purpose to describe the management of chronic ischemia.) In the emergency department it is sensible to identify and directly treat the patients with true acute leg ischemia and schedule treatment of patients with chronic disease for later. Examples of findings in medical history and physical examination are listed in Table 5 .
Table 5. Medical history and physical examination findings suggesting chronic leg ischemia
Acute Ischemia After Previous Vascular Reconstruction
A substantial number of patients have chronic leg ischemia and have undergone vascular reconstructions, so there is a high likelihood that emergency department physicians will have to take care of problems with postoperative acute leg ischemia in the operated leg. The clinical presentation of graft failure or occlusion is variable. An abrupt change in leg function and skin temperature accompanied by the onset of pain can occur any time after surgery, but especially within the first 6 months. Several years after the reconstruction it is slightly more common for progressive deterioration to occur and an eventual graft occlusion to pass unnoticed. As discussed previously in this chapter the management principles are roughly the same as for primary acute leg ischemia. It is the status of the leg and the severity of ischemia that lead workup and management. Most patients will undergo angiography to establish diagnosis and to provide information about possibilities to restore blood flow. Thrombolysis is often the best treatment option because it exposes the underlying lesions that may have caused the occlusion. As for patients with acute ischemia, those with an immediately threatened leg after a reconstruction should be taken to the operating room and treated as fast as possible.
Date: 2014-12-29; view: 884
|