
CATEGORIES:
BiologyChemistryConstructionCultureEcologyEconomyElectronicsFinanceGeographyHistoryInformaticsLawMathematicsMechanicsMedicineOtherPedagogyPhilosophyPhysicsPolicyPsychologySociologySportTourism
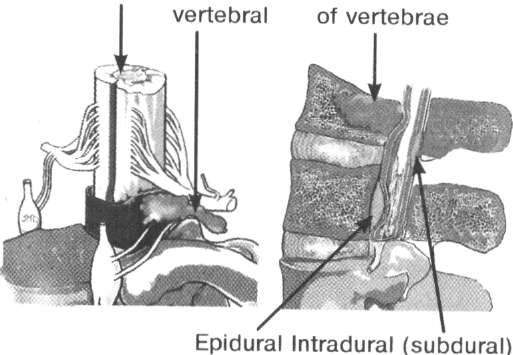
Tumours of the spinal cordTumours of spinal cord (SC) make 10-15% of all tumours of CNS and occur with the same frequency in men and women at the age from 20 to 60 years. They classify the tumours of SC by histogenesis, localization, degree of malignancy. By a histological structure they distinguish tumours which develop from tissues of the spinal cord -astrocytomas, ependymomas, glioblastomas, oligodendrogliomas and others, from vessels - angiomas, from membranes - meningiomas, from the roots of SC - neurinomas, from connective tissue elements - sarcomas, from adipose tissues - lipomas. Depending on localization, tumours of the spinal cord are divided into extramedullar which develop from the membranes of the spinal cord, its roots and nearby tissues surrounding the spinal cord, and intramedullar which arise from cellular elements of the spinal cord. In turn, extramedullar tumours are divided into subdural (intradural), which are located under the dura mater of the SC, epidural (extradural) - over the dura mater of SC, and epi-subdural. By their relation to the vertebral canal tumours of the spinal cord are divided into intravertebral (within the limits of the vertebral canal), extravertebral, extra- intravertebral (like the sand-glass - Gulike's tumours; Fig. 1). Fig. 1. Types of tumours of the spinal cord depending on their location In relation to the length of the spinal cord they distinguish tumours of the cervical, thoracic, lumbar parts, tumours of the cauda equina. More than in half of cases tumours occur in the cervical and lumbar parts. In the cervical part tumours of the spinal cord in children occur twice more frequently than in elderly persons, and in the thoracic part of the spine - they are revealed three times more frequently in elderly people than in children. The tumours of the cauda equina are diagnosed approximately in one-fifth of patients. In children, more characteristically is formation of lipomas, dermoid cysts, sarcomas, epidural ependymomas. Middle-aged persons have neurinomas more frequently, and rarer-meningiomas. In people of advanced age, they diagnose meningiomas, neurinomas, metastases of cancer. They also distinguish craniospinal tumours: they spread from the cranial cavity into the vertebral canal or vice versa. To the extramedullar tumours of the spinal cord belong: 1. meningiomas (arachnoid endotheliomas) which originate from brain membranes; 2. neurinomas which develop from Schwann's cells of mainly posterior roots of the spinal cord; 3. vascular tumours (hemangioendotheliomas, hemangioblastomas, angiolipomas, angiosarcomas, angioreticulomas - well vascularized tumours, in particular cases multiple neoplasms (Gippel-Lindau's disease): 4. lipomas and other, depending on the histostructure, neoplasms. Approximately 50% of extramedullar tumours of the spinal cord are made up by meningiomas (arachnoendotheliomas) which in most cases are located subdurally. Meningiomas belong to the tumours of the mesenchimal origin, they develop from brain membranes or their vessels. They are densely connected with the dura mater of the SC. Sometimes meningiomas are calcified (psammomas). Neurinomas are observed in 1/3 of patients. They develop from Schwann's cells of the posterior roots of the spinal cord, therefore they are also named schwannomas. Neurinomas are tumours of dense consistency, an oval form, surrounded by a thin capsule. Numerous neurinomas are characteristic of Reklinghausen's disease. Tumours of heterotopical origin (dermoid cysts, epidermoids, teratomas) are diagnosed mainly in children in the first years of life. Chondromas, chordomas, chondrosarcomas belong to rarely occurring neoplasms localized mainly in the sacral part. A special group in a clinical plan is made by the tumours of the cauda equina which become apparent mainly by radicular syndromes. Intramedullar tumours of the spinal cord are presented mainly by gliomas (astrocytomas, ependymomas and others). Rarer are multiform glioblastomas, medulloblastomas, oligodendrogliomas. Intramedullar tumours develop mainly from the gray substance of the spinal cord and belong to malignant tumours with an infiltration growth. Macroscopically in the area of localization of an intramedullar tumour, the spinal cord is fusiformly thickened. Ependymomas are diagnosed mainly in patients of30-40 years and in children of school age. They are localized most frequently in the cervical part and in the area of the cauda equina, they can spread over two, three and more segments. Astrocytomas are relatively benign forms of intramedullar tumours, they occur most frequently in children of 2-5 years and are localized mainly in the cervicothoracic part of SC.
Fig. 2. The most widespread localizations of metastatic tumours of the spine and spinal cord
Of all the tumours of the spinal cord characteristic is a progradient course of disease as a result of a progressive compression of the spinal cord and damage of its roots, at that the speed of progress of neurological symptomatology depends on the localization of the tumour, direction of growth, histogenesis. The most frequent localization of tumours depending on their hyperstructure is presented in Fig.3.
Fig. 3. Dependence of localization of tumours of the spinal cord on their histological structure
The clinical picture of tumours of the spinal cord becomes apparent by syndromes: The radiculo-membraneous pain syndrome. Most characteristic of extramedullar tumours. Depending on which of the roots is damaged (anterior or posterior), there arise pains along the root, sensitiveness is disturbed. At extramedullar tumours a radicular pains increases in a horizontal position (Razdolsky's symptom), especially if the tumour is located in the area of the cauda equina, and subside in a vertical one. It has an important differential-diagnostic significance because at some diseases, for example, at tuberculous spondylitis, the pain subsides in a horizontal position of the patient. Not of minor importance is also the symptom of the spinal process: painfulness at percussion of spinal processes and paravertebrally at the level of the pathological process. The Neri's sign is characterized by strengthening a local pain syndrome at the inclination of the head forwards. Of neuromas characteristic is the CSF push symptom - the arise or strengthening of the radicular pain at compression of jugular veins. At that the outflow of venous blood from the brain gets worse, intracranial pressure grows quickly, and the wave of neurolymph spreads along the subarachnoid spaces of the spinal cord, effecting the tumour as a push with the tension of the root due to which there arises or increases the pain syndrome. Reflexes whose arcs of pass through the damaged root or lock at the level of the damaged segment, go down or disappear at the objective checkup of the patient. Therefore, the level of location of the tumour sometimes can be suspected on the basis of the prolapsed of reflex arcs - certain tendinous reflexes (peripheral paresis or paralysis).
The disturbance of sensitiveness after the radicular type becomes apparent as numbness, „crawl of small ants", feeling of cold or warmth in the area of innervation of the root. Of the radicular syndrome characteristic is the phase of irritation and the phase of prolapse of functions. In the beginning, paresthesias happen to be temporary (the phase of irritation), then - permanent. Gradually, sensitiveness in the patient goes down in the area of innervation of the root (the phase of prolapse), which in case of continuing damage of several roots, results in the development of anaesthesia (the absence of sensitiveness) in the corresponding dermatoms. The syndrome of damage of the diameter of the spinal cord. It is related to appearance of conductive and segmentary symptomatology according to the level of compression of the spinal cord. At proceeding growth of the tumour and compression of the spinal cord, there appear symptoms of damage of the spinal cord after the conductive type below the level of damage with a gradual growth of neurological symptomatology. There is the so-called syndrome of damage of the diameter of the spinal cord as disorder of motor, sensitive and vegetative functions after the central type below the level of damage. In patients there appear pareses or paralyses after the central type (spastic). The main signs of central paresis are: an increase of the muscle tone, an increase of tendinous and periosteal reflexes, the appearance of pathological pyramid reflexes (as a result of disorder of an inhibitory influence of the cortex and strengthening of reflex activity of the segmentary apparatus of the spinal cord). Cutaneous, abdominal, cremaster and other reflexes, just on the contrary, disappear, that has an important topico-diagnostic significance. Disturbances of sensitiveness become apparent as hyperpathies, hypesthesias, anaesthesias below the level of damage. Sensitive disorders are progressive after the conductive type. At extramedullar tumours one observes a characteristic ascending type of disorder of sensitiveness - from distal parts of the body (foot, perineum) with a gradual distribution of sensitive disorders upwards up to the level of the focus of damage, that is explained by a gradual compression of conductive tracts of the spinal cord from outside, where the longest fibres are located which innervate distal parts of the body. At intramedullar tumours - on the contrary, a descending type of disorder of sensitiveness develops, that is explained by the law of an eccentric location of conductors (Flatau's law). The syndrome of disorder of vegetative functions becomes apparent primarily as dysfunctions of the pelvic organs (the perineoanal syndrome). At tumours located above sympathetic (LI-LII) and parasympathetic (SIII-SV) centers of regulating of the pelvic organs located higher, in the beginning there are imperative urges to urination, then uroschesis develops in the patient. There arise the so-called paradoxical ischuria (excretion of urine by drops). At intramedullar tumours of the spinal cord at the early stages of development, there is a clinical symptomatology of damage of certain segments of the spinal cord (the segmentary type) that becomes apparent by hyperpathies, sympathalgia in the area of the damaged segments. There appear fibrillar twitches of muscles, disorders of sensitiveness after the dissociated type (prolapse of superficial types at the persistence of deep types of sensitiveness). In future, there becomes apparent symptomatology of damage of the spinal cord after the peripheral type (oligoatrophy of muscles, hypotonus). As the tumour grows, the spinal cord is destructed from the inside and it is thickened fusiformly, symptoms of damage of the spinal cord join after the conductive type as a result of compression of conductive tracts of the spinal cord to the walls of the vertebral canal. In this period, the clinic of damage of the spinal cord is of a mixed nature - the symptoms of damage of the segmentary apparatus are joined by the symptoms of pyramid insufficiency of the spinal cord, there appears symptomatology of damage of the spinal cord appears after the central type (tendinous and periosteal reflexes increase, pathological pyramid signs appear, conductive cacesthesias progress). At that, atrophy of certain groups of muscles of the upper extremities is saved. The clinical picture of the tumour of the spinal cord depends on its localization. At tumours of the cervical part of the spinal cord at the level of CI-CIII segments there arises a radicular pain in the cervical area with the limitation of the volume of motions in the cervical part of the spine. Central tetraparesis (tetraplegia) grows, sensitive disorders progress in the upper and lower extremities. At localization of tumour at the level CIV of segment there joins disturbance of breathing because of damage of the diaphragmatic nerve (phrenoplegia). At craniospinal tumours there can be clinical symptomatology of intracranial hypertension with stagnation on the ocular fundus, at the damage of medulla oblongata - bulbar disorders. Of the damage of CV-ThI segments characteristic is the development of flaccid peripheral paresis of the upper extremities and central lower paraparesis, which in the course of time turns into the lower paraplegia. At compression by tumour of the ciliospinal center (CVIII-DI), Bemard-Horner's syndrome (ptosis, myosis, enophthalmos) or its elements develop. Function of V and IX pairs of craniospinal nerves can be disordered. In tumours of the thoracic part of the spinal cord, along with the syndrome of damage of the diameter of the spinal cord as disorders of motor, sensitive, and vegetative functions after the central type below the level of damage, there can arise a radicular pain along the intercostal nerves. Disturbance of cardiac activity can be observed at localization of tumour at the level of Th2 -Th6 segments. In damage of the lower thoracic segments there arise a pain in the area of the stomach, that can result in the misbelief about the presence of cholecystitis, pancreatitis or appendicitis in the patient. Of tumours in the area of ThVII-ThVIII characteristic is the absence of abdominal reflexes, at tumours in ThIX-ThX - the absence of middle and lower abdominal reflexes, of damage of segments of ThXI-ThXII - the absence of lower abdominal reflexes only is characteristic. In tumour at the level of the lumbar thickening (LI-SII), in the patient there develops a lower flaccid paraplegia or paraparesis develops with absence of reflexes and atony of muscles of the lower extremities, the function of the pelvic organs is disordered. At localization of the tumour at the level of the upper part of the thickening, knee-jerks reflexes are not caused or decreased, the Achilles ones - increased. In tumour at the level of the lower segments of the lumbar thickening, knee-jerks reflexes are saved, foot ones are decreased or not caused. Of the damage of epiconus (LIV-SII) characteristic is the appearance of flaccid paresis of feet flexors and extensors, muscles of the peroneal group, sciatic muscles at the persistence of knee-jerks and loss of the Achilles reflexes. Tumours in the area of the cerebral cone are characterized by pains in the area of the perineum and in the anogenital area. At the damage by the tumour of parasympathetic centers, there are dysfunctions of the pelvic organs after the peripheral type (incontinence of urine and stool, sexual impotence). Tumours in the area of the cauda equina manifest themselves by an apparent pain in the sacrum, anogenital area, in the lower extremities which increase in a horizontal position, especially at night. Motor and sensitive disorders progress in the lower extremities after the radicular type, the function of the pelvic organs is disordered after the type of incontinence.
Date: 2015-02-16; view: 1277
|
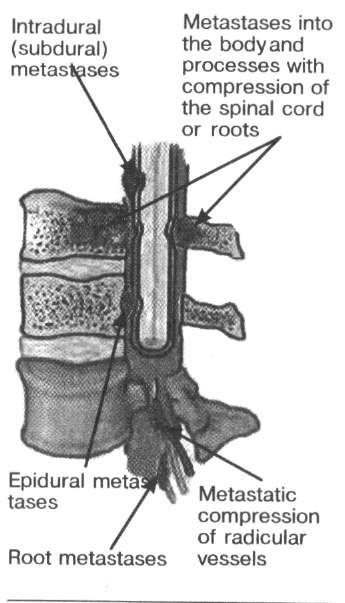 Metastatic tumours occur in 1% of cases. As a rule, they penetrate through the venous system of the spine. Such metastases spread from the mammary gland, prostate, lungs, organs of GIT (gastrointestinal tract), kidneys. These tumours grow quickly, destroy the bone tissue of the spine, ligamentous apparatus and soft tissues, causing the compression of the spinal cord with an apparent pain syndrome. In Fig.2, the most frequent localization of metastatic tumours is presented.
Metastatic tumours occur in 1% of cases. As a rule, they penetrate through the venous system of the spine. Such metastases spread from the mammary gland, prostate, lungs, organs of GIT (gastrointestinal tract), kidneys. These tumours grow quickly, destroy the bone tissue of the spine, ligamentous apparatus and soft tissues, causing the compression of the spinal cord with an apparent pain syndrome. In Fig.2, the most frequent localization of metastatic tumours is presented.